Biomedical Engineering Theory And Practice/Biomechanics
Classical Mechanics
[edit | edit source]See also Wikipedia,List of equations in classical mechanics
Rigid Body Mechanics
[edit | edit source]Rigid body defined as a body on which the distance between any two given points remains constant in time regardless of external forces[1]. Or it is the body which does not deform under the influence of forces[1].Forces acting of rigid bodies can be also separated in two groups: The external forces, represent the action of other bodies on the rigid body under consideration; The internal forces are the forces which hold together the particles forming the rigid body. The body is only able to change its motion if it can push or pull against some external object. Only external forces can impart to the rigid body a motion. Rigid body makes analysis simple with less parameters that describe the configuration of the system to the translation and rotation of reference frames attached to each body.[2][3]Rigid-body mechanics studies the movement of interconnected bodies' system under the action of external forces.
Kinematics
[edit | edit source]Kinematics describes the motion of points, bodies (objects) and systems of bodies (groups of objects) without consideration of the causes of motion. It is the branch of biomechanics concerned with the study of movement from a geometrical point of view.[4][5][6]
Type of Motions
[edit | edit source]Motions are classified into translation and rotation according to a fixed axis, general plane motion and motion about a fixed pin.
- Translation(Linear Motion):A motion is said to be a translation if any straight line inside the body keeps the same direction during the movement. All the particles forming the body move along parallel paths. If these paths are straight lines, the motion is said a rectilinear translation. If the paths are curved lines, the motion is a curvilinear motion.
- Rotation about a fixed axis(Angular Motion): Most of the individual limb motions are angular. The particles forming the rigid body move in parallel planes along circles centered on the same fixed axis. If this axis, called the axis of rotation intersects the rigid body, the particles located on the axis have zero velocity and zero acceleration.
- General plane motion: Any plane motion which is neither a translation or a rotation is defined as a general plane motion. Plan motion is that in which all the particles of the body move in parallel planes. Translation and rotation are plane motions.
- Motion about a fixed point: The three-dimensional motion of a rigid body attached at a fixed point, for example, the motion of a top on a rough floor, is known as motion about a fixed point.
- General motion: Any motion of a rigid body which does not fall in any of the categories above described.
Position
[edit | edit source]Position(also called Displacement) means an object’s location at any particular time.
Velocity
[edit | edit source]Velocity is defined as the rate at which location changes with time.
Acceleration
[edit | edit source]Acceleration is the rate at which velocity changes with time.
Kinetics
[edit | edit source]Kinetics is the branch of biomechanics concerned with what causes a body to move the way it does.
Newton’s Laws of Motion
[edit | edit source]Newton's laws of motion are three fundamental laws for classical mechanics. They describe the relationship between a body and the forces acting upon it, and its motion to the forces.
- Newton's first law: If a body is at rest it remains at rest or if it is in motion it moves with uniform velocity until it is acted on by a resultant force.[7]The first law can be stated mathematically as ⇔
- Newton's second law: Acceleration is dependent on the forces acting upon an object and the mass of the object. Change in momentum is proportional to external force and reversely proportional to its mass. It can be stated mathematically as .To consider rigid body three-dimensionally, Newton's second law should be extended to define the relationship between the movement of a rigid body and the system of forces and torques that act on it.
- Newton's third law: For all force, there is an equal and opposite force. If one object A exerts a force FA on a second object B, then B simultaneously exerts a force FA on A: FA= −FA[8].
Molecular Biomechanics
[edit | edit source]Biomolecules and intermolecular forces
[edit | edit source]
Single molecule biopolymer mechanics
[edit | edit source]Formation and dissolution of bonds
[edit | edit source]Motion at the molecular/macromolecular level
[edit | edit source]Tissue Mechanics I (Bone)
[edit | edit source]Microscopic bone structure
[edit | edit source]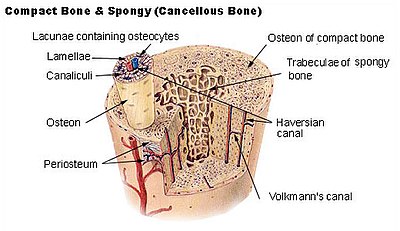
Two types of bone can be founded microscopically up to the pattern of collagen forming the osteoid (collagenous support tissue of type I collagen embedded in glycosaminoglycan gel):
- Woven bone is characterized by randomly oriented collagen fibers. It is isotropic and mechanically weak[9]. It is actively resolved by 1 year.
- Lamellar bone has a highly organized parallel alignment of collagen into sheets (lamellae). It is anisotropic and mechanically strong [9].
Bone Tissue: Cortical (Compact) Bone
[edit | edit source]Cortical bone, also called compact bone, dense bone in which the bony matrix is solidly filled with collage and Hydroxylapatite, leaving only tiny spaces (lacunae) that contain the osteocytes, or bone cells.[10]Its porosity is 5–30%.[11] Compact bone makes up 80 percent of the human skeleton. Cortical bone forms the cortex, or outer shell, of most bones[10] .
Bone Tissue: Trabecullar (Cancellous or spongy) Bone
[edit | edit source]Compared to compact bone, cancellous bone has a higher surface area to mass ratio because it is less dense. It's porosity is %30-90[11]. It is composed of a network of rod- and plate-like elements that make the overall organ lighter and allow room for blood vessels and marrow where haematopoiesis, the production of blood cells, occurs. Cancellous bone is typically found at the ends of long bones, proximal to joints and within the interior of vertebrae.
Bone Tissue Type and Implant
[edit | edit source]- Type I bone is very hard and dense like oak wood as it contains mostly lamellae bone. This type of bone has less blood supply than all of the rest of the types of bone. The blood supply is required for the bone to harden or calcify the bone for the implant. Therefore, it needs approximately 5 months for this type to integrate with an implant[12].
- Type II plexiform bone isn't as hard as type I. It is composed of layers of lamellae and woven bone. This type of bone usually takes 4 months to integrate with an implant[12]
- Type III Haversian bone is composed of Harversian canal, concentric lamellae, lacunae with osteocytes and canaliculi. It is like balsa wood and less dense then type II. Because of lower density, it takes more time to work with an implant. 6 months time is suggested before loading an implant placed in this bone. Extended gradual loading of the implant could improve the bone density[12].
- Type IV cancellous bone is the least dense of all of the bone types[11].This type takes the longest time to work with the implant after placement, which is usually 8 months. Additional implants is necessary to improve implant/bone loading distribution. Bone grafting or augmentation of bone are often needed. Bone expansion and or bone manipulation can improve initial implant fixation[12].
Bone Cells
[edit | edit source]
Bone cells are classified into four categories: osteoclasts destroy bones, osteoblasts build bones, osteocytes hold the bone together and, lining cells protect the bone.
osteoclast
[edit | edit source]Osteoclasts are usually found in bone surface called resorptive pits. Osteoclasts are large multinucleate cells that are responsible for the breakdown of bones[13]. The breakdown of bone is very important in bone health as it allows for bone remodeling. Osteoclasts are formed by the joining of many different cells created from the bone marrow that travel in the circulatory system[13]. Local acidic environment through H2 enhance the solubility of hyaluronic acid. High molecular weight hyaluronic acid regulates osteoclast formation by inhibiting receptor activator of NF-κB ligand through Rho kinase[14].
osteoblasts
[edit | edit source]Osteoblasts is primarily composed of Type I collagen. The osteoblast creates and repairs new bone by actually building around itself. After the osteoblast is finished working, it is actually trapped inside of the bone. When the osteoblast becomes trapped, it becomes known as an osteocyte[15]
osteocytes
[edit | edit source]Osteocytes are mature osteoblasts which have become trapped inside of lacunae surrounded by bone matrix. The osteocytes are numerous and believed to communicate with stress/strain signal[16].
lining cells
[edit | edit source]Bone lining cells come from osteoblasts which have become flattened. Bone lining cells are for the immediate release of calcium] in the bone if calcium in the blood is too low. Bone lining cells are also important in the protection of the bone from harmful chemicals. And bone lining cells are responsible for the maintenance of the bone fluids[17].
Biomechanical Behaviour of Bone
[edit | edit source]Cortical Bone
[edit | edit source]It has relatively high compressive strength of about 170 MPa (1800 kgf/cm2)[18] but poor tensile strength of 104–121 MPa and very low shear stress strength (51.6 MPa)[19].
Trabecular Bone
[edit | edit source]Elastic behaviours depends on the anatomic sites, age, connectivity and so on. Modulus and strength are weak dependent on the strain rate[20]
Tissue Mechanics II (Cartilage, Muscle, Ligament, Tendon)
[edit | edit source]
All connective tissue including bone and adipose is characterized by distinctive cells surrounded by an extracellular matrix within a ground substance. The tissue is characterized based on the extracellular matrix. Blood is also belong to the connective tissue. Special connective tissue consists of reticular connective tissue, adipose tissue, cartilage, bone, and blood.[21]
Cartilage
[edit | edit source]Cartilage is a flexible and rubbery but strong supportive connective tissue[22] Cartilage consists of cells called chondrocytes which are dispersed in a firm gel-like ground substance and produce and maintain the cartilaginous matrix composed mainly of collagen and proteoglycans. Cartilage is avascular (contains no blood vessels) and nutrients are diffused through the matrix. Cartilage is found in many areas in the bodies of humans and other animals, including the joints between bones, the rib cage, the ear, the nose, the bronchial tubes and the intervertebral discs.
There are three main types of cartilage: hyaline, elastic and fibrocartilage[23].
Hyaline cartilage
[edit | edit source]The type of protein fiber embedded within the matrix of cartilage determines the cartilage type[24]. It contains no nerves or blood vessels, and its structure is relatively simple. Hyaline cartilage matrix is mostly composed of type II collagen and chondroitin sulfate, both of which are also found in elastic cartilage. The optical density of these fibers is the same as the ground substance surrounding them and as a result, they are not visible within the extracellular matrix. Hyaline cartilage subsequently appears as a very uniform, glossy type tissue with evenly dispersed chondrocytes in lacunae. Typically, hyaline cartilage is covered by the perichondrium, except at the articular ends of bones. It is found directly under the skin, i.e. ears and nose. This membrane contains vessels that provide the cartilage with nutrition.
Articular cartilage indicates hyaline cartilage on the articular surfaces of bones.[25][26]
Elastic cartilage
[edit | edit source]Elastic cartilage or yellow cartilage is found in the pharyngotympanic (eusatachian) tubes, epiglottis, and ear lobes where needs dictate supportive tissues possess elasticity. It contains elastic fiber networks and collagen fibers.[27] The principal protein is elastin.
Fibrocartilage
[edit | edit source]Fibrocartilage (fibrous) contains type I collagen in addition to the normal type II arranged in layered arrays. compared to the very uniform appearance of hyaline cartilage, fibrocartilage possesses a more open or spongey architecture with gaps between lacunae and collagen fiber bundles. Fibrocartilage is found in the pubic symphysis, the annulus fibrosus of intervertebral discs, menisci, and the TMJ. It helps fill in the torn part of the cartilage; but, it is not enough for the replacement of the smooth, glassy articular cartilage that normally covers the surface of joints. The tendon transforms into fibrocartilage when subjected to compression.[28]
Articular cartilage
[edit | edit source]Articular cartilage is the loadbearing connective tissue of diarthrodial joints[26]. Surface is a large extracellular membrane (proteoglycans, collagens, water) with a sparse population of condrocytes[29].
Along with collagen fiber ultrastructure and ECM, chondrocytes contribute to the zones of articular cartilage—the superficial zone, the middle zone, the deep zone, and the calcified zone. Collagen is main structural macromolecule in ECM, and it occupy about 60% of the dry weight of cartilage. Type II collagen represents 90% to 95% of the collagen in ECM and forms fibrils and fibers intertwined with proteoglycan aggregates together along hyaluronic acid core. Collagen types I, IV, V, VI, IX, and XI also exist but contribute only a minor proportion. The minor collagens help to form and make the type II collagen fibril network stable. Water represents between 65% and 80% of the total weight.The relative water concentration decreases from about 80% at the superficial zone to 65% in the deep zone[30].Water and proteoglycans are critical to its ability to resist compressive loads.
Its principal function is to provide a smooth, lubricated surface for articulation and to facilitate the transmission of loads with a low frictional coefficient. The mechanical behavior of this tissue is dependent on the interaction of its fluid and solid components[26].
Ligament and Tendon
[edit | edit source]A tendon is a tough fibrous bands of connective tissue that usually attaches muscle to bone. Tendons may also connect muscles to structures such as the eyeball. A tendon serves to move the bone or structure. A ligament is a short, fibrous bands of connective tissue which attaches bone to bone, and usually serves to hold structures together and stabilize them[31]. Ligament and tendon are different in the connection to the system. But, ligament and tendon are dense connective tissue and microscopically similar to including composition.
Muscle Tissue
[edit | edit source]
Muscle Tissue is a band or bundle of fibrous tissue in a human or animal body that has the ability to contract, producing movement in or maintaining the position of parts of the body. Muscle (myocytes) are elongated cells ranging from several millimeters to about 10 centimeters in length and from 10 to 100 micrometers in width.[32]. According to the function and location in the body, muscle tissue is divided into three: skeletal muscle, cardiac muscle and smooth muscle. Cardiac and skeletal muscles are "striated" as they include sarcomeres and are packed into highly regular arrangements of bundles; smooth muscle is not. While skeletal muscles are arranged in regular, parallel bundles, cardiac muscle connects at branching, irregular angles (called intercalated discs). Skeletal muscle is under the control of the somatic nervous system. In other words, it is voluntarily controlled. Cardiac muscle (heart muscle) is involuntary striated muscle in the walls of the heart, specifically the myocardium.
Comparison of Muscle Tissue[33]
[edit | edit source]Cellular Biomechanics
[edit | edit source]Structure/function/properties of the cell
[edit | edit source]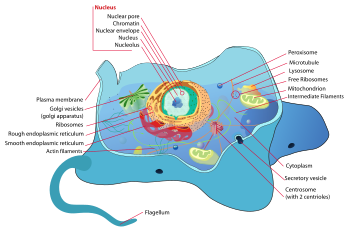
Cell membranes
[edit | edit source]
The cytoskeleton[34]
[edit | edit source]| Cytoskeleton type[35] | Diameter (nm)[36] | Structure | Subunit examples[35] | Persistence Length (µm) |
|---|---|---|---|---|
| Microfilaments | 6 | double helix | actin | 15 |
| Intermediate filaments | 10 | two anti-parallel helix/dimers, forming tetramers |
|
1-3 |
| Microtubules | 23 | protofilaments, in turn consisting of tubulin subunits in complex with stathmin[37] | α-bubulin and β-tubulin | 60,000 |
Cell adhesion and aggregation
[edit | edit source]Cell adhesion is the process by which cells interact and attach to neighbouring cells through specialised molecules of the cell surface. This process can occur either through direct contact between cell surfaces such as cell junctions or indirect interaction, where cells attach to surrounding extracellular matrix, a gel-like structure containing molecules released by cells into spaces between them. Cells adhesion occurs from the interactions between cell-adhesion molecules (CAMs), transmembrane proteins located on the cell surface. Cell adhesion links cells in different ways and can be involved in signal transduction for cells to detect and respond to changes in the surroundings. Other cellular processes regulated by cell adhesion include cell migration and tissue development in multicellular organisms. Alterations in cell adhesion can disrupt important cellular processes and lead to a variety of diseases, including cancer and arthritis. Cell adhesion is also essential for infectious organisms, such as bacteria or viruses, to cause diseases.
Cell migration
[edit | edit source]Cell migration is a central process in the development and maintenance of multicellular organisms. Tissue formation during embryonic development, wound healing and immune responses all require the orchestrated movement of cells in particular directions to specific locations. Cells often migrate in response to specific external signals, including chemical signals and mechanical signals. Errors during this process have serious consequences, including intellectual disability, vascular disease, tumor formation and metastasis. An understanding of the mechanism by which cells migrate may lead to the development of novel therapeutic strategies for controlling, for example, invasive tumour cells.
Due to the highly viscous environment (low Reynolds number), cells need to continuously produce forces in order to move. Cells achieve active movement by very different mechanisms. Many less complex prokaryotic organisms (and sperm cells) use flagella or cilia to propel themselves. Eukaryotic cell migration typically is far more complex and can consist of combinations of different migration mechanisms. It generally involves drastic changes in cell shape which are driven by the cytoskeleton. Two very distinct migration scenarios are crawling motion (most commonly studied) and blebbing motility. A paradigmatic example of crawling motion is the case of fish epidermal keratocytes, which have been extensively used in research and teaching.
Mechanotransduction
[edit | edit source]Mechanotransduction (mechano + transduction) is any of various mechanisms by which cells convert mechanical stimulus into electrochemical activity. This form of sensory transduction is responsible for a number of senses and physiological processes in the body, including proprioception, touch, balance, and hearing. The basic mechanism of mechanotransduction involves converting mechanical signals into electrical or chemical signals.
In this process, a mechanically gated ion channel makes it possible for sound, pressure, or movement to cause a change in the excitability of specialized sensory cells and sensory neurons. The stimulation of a mechanoreceptor causes mechanically sensitive ion channels to open and produce a transduction current that changes the membrane potential of the cell. Typically the mechanical stimulus gets filtered in the conveying medium before reaching the site of mechanotransduction. Cellular responses to mechanotransduction are variable and give rise to a variety of changes and sensations. Broader issues involved include molecular biomechanics.
Further Reading
[edit | edit source]- Bronzino, Joseph D. (April 2006). The Biomedical Engineering Handbook, Third Edition. [CRC Press]. ISBN 978-0-8493-2124-5.
- Villafane, Carlos, CBET. (June 2009). Biomed: From the Student's Perspective, First Edition. [Techniciansfriend.com]. ISBN 978-1-61539-663-4.
{{cite book}}: CS1 maint: multiple names: authors list (link) - Information related to biomedical engineering.
Practise
[edit | edit source]6.1 A very brief review of basic mechanics: Vectors and kinematics, Force and Motion, Kinetic and Potential Energy and Work, Conservation of Energy, Energy Absorption, Center of Mass and Linear & Angular Momentum, Rotation, Torque, and Elasticity,Axial Stress and Strain Shear Stress, Bending, Torsion,Failure Under Load,
6.2 Cellular Biomechanics
6.3 Mechanics of Hard &Soft Tissue Tissues
6.4.1 mechanics of the Musculoskeletal & digestive systems
6.4.2 Joint Surface & Lubrication
Reference
[edit | edit source]- ↑ a b http://makox.com/mechanical-engineering/what-is-a-rigid-body/
- ↑ B. Paul, Kinematics and Dynamics of Planar Machinery, Prentice-Hall, NJ, 1979
- ↑ L. W. Tsai, Robot Analysis: The mechanics of serial and parallel manipulators, John-Wiley, NY, 1999.
- ↑ Edmund Taylor Whittaker (1904). A Treatise on the Analytical Dynamics of Particles and Rigid Bodies. Cambridge University Press. Chapter 1. ISBN 0-521-35883-3.
- ↑ Joseph Stiles Beggs (1983). Kinematics. Taylor & Francis. p. 1. ISBN 0-89116-355-7.
- ↑ Thomas Wallace Wright (1896). Elements of Mechanics Including Kinematics, Kinetics and Statics. E and FN Spon. Chapter 1.
- ↑ Duncan, Tom. Advanced Physics for Hong Kong: Volume 1 Mechanics & Electricity. John Murray Ltd, 1995
- ↑ Resnick; Halliday; Krane (1992). Physics, Volume 1 (4th ed.). p. 83.
- ↑ a b Curry, J.D. 2006. "The Structure of Bone Tissue" Bones: Structure and Mechanics Princeton U. Press. Princeton, NJ. pps: 12–14
- ↑ a b Encyclopedia Britanica,compact bone
- ↑ a b c Hall, Susan. (2007) Basic Biomechanics. Fifth Edition. p. 88 ISBN 0-07-126041-2
- ↑ a b c d http://www.americanortho.com/downloads/aarhus/Bone_types.pdf
- ↑ a b H. Kalervo Väänänen et al,Journal of Cell Science 113, 377-381 (2000)
- ↑ Ariyoshi W et al. Osteoarthritis Cartilage. 2014 Jan;22(1):111-20
- ↑ Davis, Michael. "DrTummy.com | DrTummy.com." DrTummy.com | DrTummy.com. Dr. Tummy, n.d. Web. 03 Apr. 2013.
- ↑ "Bone Cells." ASBMR Educational Materials. N.p., n.d. Web. 08 Apr. 2013.
- ↑ "Bone Cells." ASBMR Educational Materials. N.p., n.d. Web. 08 Apr. 2013.
- ↑ Schmidt-Nielsen, Knut (1984). "Scaling: Why Is Animal Size So Important?". Cambridge: Cambridge University Press: 6. ISBN 0-521-31987-0.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Turner, C.H.; Wang, T.; Burr, D.B. (2001). "Shear Strength and Fatigue Properties of Human Cortical Bone Determined from Pure Shear Tests". Calcified Tissue International. 69 (6): 373–378. doi:10.1007/s00223-001-1006-1. PMID 11800235.
- ↑ Goldstein SA. J. Biomech. 1987;20(11-12):1055-61
- ↑ Caceci, Thomas. "Connective Tisues". Retrieved 9 December 2012.
- ↑ Tissues of the human body McGrawHill
- ↑ Pratt, Rebecca. "Supporting Tissue: Cartilage". AnatomyOne. Amirsys, Inc. Retrieved 26 October 2012.
- ↑ Britanica, Hyaline cartilage
- ↑ [1]
- ↑ a b c Alice J. Sophia Fox, MSc Sports Health. Nov 2009; 1(6): 461–468.
- ↑ emedicine health,elastic cartilage
- ↑ [http://www.wheelessonline.com/ortho/12642 Wheeless' Textbook of Orthopaedics ]
- ↑ Mow VC, Ratcliffe A, Poole AR. Cartilage and diarthrodial joints as paradigms for hierarchical materials and structures. Biomaterials. 1992;13:67-97
- ↑ Buckwalter JA, Mankin HJ. Articular cartilage, part 1: tissue design and chondrocyte-matrix interaction. J Bone Joint Surg Am. 1997;79:600-611
- ↑ MedlinePlus
- ↑ Hugh Potter, Summary of muscle tissue
- ↑ Wikipedia, Cardiac Muscle
- ↑ Wikipedia,Cytoskeleton
- ↑ a b Unless else specified in boxes, then ref is:Walter F., PhD. Boron (2003). Medical Physiology: A Cellular And Molecular Approaoch. Elsevier/Saunders. p. 1300. ISBN 1-4160-2328-3. Page 25
- ↑ Fuchs E, Cleveland DW (January 1998). "A structural scaffolding of intermediate filaments in health and disease". Science. 279 (5350): 514–9. Bibcode:1998Sci...279..514F. doi:10.1126/science.279.5350.514. PMID 9438837.
- ↑ Steinmetz MO (2007). "Structure and thermodynamics of the tubulin-stathmin interaction". J Struct Biol. 158 (2): 137–47. doi:10.1016/j.jsb.2006.07.018. PMID 17029844.