Biomedical Engineering Theory And Practice/Biomechanics II
Joint Surface Motion
[edit | edit source]Ankle
[edit | edit source]The ankle is the region where the foot and the leg meet.[1] The ankle joint is composed of three joints: the talocrural (ankle) joint and the talocalcaneal (subtalar joint) and the Inferior tibiofibular joint[2][3]. The ends of the bones in the ankle joint are covered with cartilage. The talocrural joint is formed by the articulation of the fibula and distal tibia with the trochlea of the talus. The talocalcaneal joint is formed by the articulation of the talus with the calcaneus.
Joint Contact
[edit | edit source]The talocrural joint contact area are various with flexion of the ankle.

Table. Talocalcaneal (Ankle) Joint Contact Area
| Investigators | Plantarflexion | Neutral | Dorsiflexion |
|---|---|---|---|
| Ramsey and Hamilton [1976] | 4.40 ± 1.21 | ||
| Libotte et al. [1982] | 5.01 (30o) | 5.41 | 3.60 (30o) |
| Paar et al. [1983] | 4.15 (10o) | 4.15 | 3.63 (10o) |
| Macko et al. [1991] | 3.81 ± 0.93 (15o) | 5.2 ± 0.94 | 5.40 ± 0.74 (10o) |
| Driscoll et al. [1994] | 2.70 ± 0.41 (20o) | 3.27 ± 0.32 | 2.84 ± 0.43 (20o) |
| Pereira et al. [1996] | 1.49 (20o) | 1.67 | 1.47 (10o) |
| Rosenbaum et al. [2003] | 2.11 ± 0.72 |
Axis of Rotation
[edit | edit source]Joint motion of the talocrural joint has been studied to define the axes of rotation and their location according to specific anatomic landmarks.
Table. Axis of Rotation for the Ankle
| Investigators | Axis | Position |
|---|---|---|
| Elftman [1945] | Fix. | 67.6 ± 7.4o with respect to sagittal plane |
| Isman and Inman [1969] | Fix. | 8 mm anterior, 3 mm inferior to the distal tip of the lateral malleolus; 1 mm posterior, 5 mm inferior to the distal tip of the medial malleolus |
| Allard et al. [1987] | Fix. | 95.4 ± 6.6o with respect to the frontal plane, 77.7 ± 12.3o with respect to the sagittal plane, and 17.9 ± 4.5o with respect to the transverse plane |
| Singh et al. [1992] | Fix. | 3.0 mm anterior, 2.5 mm inferior to distal tip of lateral malleolus;2.2 mm posterior, 10 mm inferior to distal tip of medial malleolus |
| Sammarco et al. [1973] | Ins. | Inside and outside the body of the talus |
| D’Ambrosia et al. [1976] | Ins. | No consistent pattern |
| Parlasca et al. [1979] | Ins. | 96% within 12 mm of a point 20 mm below the articular surface of the tibia along the long axis |
| Van Langelaan [1983] | Ins. | At an approximate right angle to the longitudinal direction of the foot, passing through the corpus tali, with a direction from anterolaterosuperior to posteromedioinferior |
| Barnett and Napier | Q-I | Dorsiflexion: down and lateral
Plantarflexion: down and medial |
| Hicks [1953] | Q-I | Dorsiflexion: 5 mm inferior to tip of lateral malleolus to 15 mm anterior to tip of medial malleolus
Plantarflexion: 5 mm superior to tip of lateral malleolus to 15 mm anterior, 10 mm inferior to tip of medial malleolus |
a Fix. = fixed axis of rotation; Ins. = instantaneous axis of rotation; Q-I = quasi-instantaneous axis of rotation.
The motion axes of the talocalcaneal joint have been described by several authors.
Table Axis of Rotation for the Talocalcaneal (Subtalar) Joint
| Investigators | Axisa | Position |
|---|---|---|
| Manter [1941] | Fix. | 16o(8–24o) with respect to sagittal plane, and 42o(29–47o) with respect to
transverse plane |
| Shephard [1951] | Fix. | Tuberosity of the calcaneus to the neck of the talus |
| Hicks [1953] | Fix. | Posterolateral corner of the heel to superomedial aspect of the neck of the talus |
| Isman and Inman [1969] | Fix. | 23o± 11owith respect to sagittal plane, and 41o± 9owith respect to transverse plane |
| Kirby [1947] | Fix. | Extends from the posterolateral heel, posteriorly, to the first intermetatarsal space,anteriorly |
| Rastegar et al. [1980] | Ins. | Instant centers of rotation pathways in posterolateral quadrant of the distal articulating tibial surface, varying with applied load |
| Van Langelaan [1983] | Ins. | A bundle of axes that make an acute angle with the longitudinal direction of the foot passing through the tarsal canal having a direction from anteromediosuperior to posterolateroinferior |
| Engsberg [1987] | Ins. | A bundle of axes with a direction from anteromediosuperior to posterolateroinferior |
aFix. = fixed axis of rotation; Ins. = instantaneous axis of rotation.
Knee
[edit | edit source]The knee joint joins the thigh with the leg and consists of the tibiofemoral articulation(one between the femur and tibia) and the patellofemoral articulation(one between the femur and patella)[4].

Table. Posterior Femoral Condyle Spherical Radius
| Normal knee | Varus knees | Valgus knees | |
|---|---|---|---|
| Medial condyle | 20.3 ± 3.4(16.1–28.0) | 21.2 ± 2.1(18.0–24.5) | 21.1 ± 2.0(17.84–24.1) |
| Lateral condyle | 19.0 ± 3.0(14.7–25.0) | 20.8 ± 2.1(17.5–30.0) | 21.1∗ ± 2.1(18.4–25.5) |
Source: Matsuda S., Miura H. Nagamine R., Mawatari T., Tokunaga M., Nabeyama R., and Iwamoto Y. Anatomical analysis of the femoral condyle in normal and osteoarthritic knees.J. Ortho. Res. 22: 104–109, 2004.


Table Geometry of the Proximal Tibia
| Parameter | Symbols | All limbs | Male | Female |
|---|---|---|---|---|
| Tibial plateau with widths (mm) | ||||
| Medial plateau | T1 | 32 ± 3.8 | 34 ± 3.9 | 30 ± 22 |
| Lateral plateau | T3 | 33 ± 2.6 | 35 ± 1.9 | 31 ± 1.7 |
| Overall width | T1+T2+T3 | 76 ± 6.2 | 81 ± 4.5 | 73 ± 4.5 |
| Tibial plateau depths (mm) | ||||
| AP depth, medial | T4 | 48 ± 5.0 | 52 ± 3.4 | 45 ± 4.1 |
| AP depth, lateral | T5 | 42 ± 3.7 | 45 ± 3.1 | 40 ± 2.3 |
| Interspinous width (mm) | T2 | 12 ± 1.7 | 12 ± 0.9 | 12 ± 2.2 |
| Intercondylar depth (mm) | T6 | 48 ± 5.9 | 52 ± 5.7 | 45 ± 3.9 |
Source: Yoshioka Y., Siu D., Scudamore R.A., and Cooke T.D.V. 1989. J. Orthop. Res. 7:132.
Table.Patellar Facet Angles
| Facet angle | 0o | 30o | 60o | 90o | 120o |
|---|---|---|---|---|---|
| γm(deg) | 60.88 | 60.96 | 61.43 | 61.30 | 60.34 |
| 3.89a | 4.70 | 4.12 | 4.12 | 4.51 | |
| γn(deg) | 67.76 | 68.05 | 68.36 | 68.39 | 68.20 |
| 4.15 | 3.97 | 3.63 | 4.01 | 3.67 |
Source: Ahmed A.M., Burke D.L., and Hyder A. 1987. J. Orthop.Res. 5: 69–85.
Joint Contact
[edit | edit source]| Knee flexion (deg) | -5 | 5 | 15 | 25 | 35 | 45 | 55 | 65 | 75 | 85 |
|---|---|---|---|---|---|---|---|---|---|---|
| Contact area (cm2) | 20.2 | 19.8 | 19.2 | 18.2 | 14.0 | 13.4 | 11.8 | 13.6 | 11.4 | 12.1 |
Source: Maquet P.G., Vandberg A.J., and Simonet J.C. 1975. J. Bone Joint Surg. 57A:766.
Table Posterior Displacement of the Femur Relative to the Tibia
| Authors | Condition | A/P displacement(mm) |
|---|---|---|
| Kurosawa [1985] | In vitro | 14.8 |
| Andriacchi [1986] | In vitro | 13.5 |
| Draganich [1987] | In vitro | 13.5 |
| Nahass [1991] | In vivo(walking) | 12.5 |
| In vivo(stairs) | 13.9 |
Axis of Rotation
[edit | edit source]Hip
[edit | edit source]
Table Geometry of the Proximal Femur
| Parameter | Females | Males |
|---|---|---|
| Femoral head diameter (mm) | 45.0 ± 3.0 | 52.0 ± 3.3 |
| Neck shaft angle (deg) | 133 ± 6.6 | 129 ± 7.3 |
| Anteversion (deg) | 8 ± 10 | 7.0 ± 6.8 |
Source: Yoshioka Y., Siu D., and Cooke T.D.V. 1987. J. Bone Joint Surg. 69A: 873.
Joint Contact
[edit | edit source]Axis of Rotation
[edit | edit source]Shoulder
[edit | edit source]

Joint Contact
[edit | edit source]Table.Glenohumeral Contact Areas
| Elevation angle (o) | Contact areas at SR (cm2 ) | Contact areas at 20ointernal to SR (cm2) |
|---|---|---|
| 0 | 0.87 ± 1.01 | 1.70 ± 1.68 |
| 30 | 2.09 ± 1.54 | 2.44 ± 2.15 |
| 60 | 3.48 ± 1.69 | 4.56 ± 1.84 |
| 90 | 4.95 ± 2.15 | 3.92 ± 2.10 |
| 120 | 5.07 ± 2.35 | 4.84 ± 1.84 |
| 150 | 3.52 ± 2.29 | 2.33 ± 1.47 |
| 180 | 2.59 ± 2.90 | 2.51 ± NA |
SR = starting external rotation which allowed the shoulder to reach maximal elevation in the scapular plane (≈40o ±8o); NA = not applicable. Source: Soslowsky L.J., Flatow E.L., Bigliani L.U.,Pablak R.J., Mow V.C., and Athesian G.A. 1992. J. Orthop.Res. 10: 524.
Axis of Rotation
[edit | edit source]Table Arm Elevation: Glenohumeral–Scapulothoracic Rotation
| Investigator | Glenohumeral/scapulothoracic
motion ratio |
|---|---|
| Inman et al. [1994] | 2:1 |
| Freedman and Munro [1966] | 1.35 : 1 |
| Doody et al. [1970] | 1.74 : 1 |
| Poppen and Walker [1976] | 4.3 : 1 (<24o elevation)
1.25 : 1 (>24oelevation) |
| Saha [1971] | 2.3 : 1 (30–135oelevation) |
Elbow
[edit | edit source]Table. Elbow Joint Geometry
| Parameter | Size (mm) |
|---|---|
| Capitulum radius | 10.6 ± 1.1 |
| Lateral trochlear flange radius | 10.8 ± 1.0 |
| Central trochlear groove radius | 8.8 ± 0.4 |
| Medial trochlear groove radius | 13.2 ± 1.4 |
| Distal location of flexion/extension
axis from transepicondylar line: | |
| Lateral | 6.8 ± 0.2 |
| Medial | 8.7 ± 0.6 |
Source: Shiba R., Sorbie C., Siu D.W., Bryant J.T.,Cooke T.D.V., and Weavers H.W. 1988. J. Orthop.Res. 6: 897.
Joint Contact
[edit | edit source]Table.Elbow Joint Contact Area
Axis of Rotation
[edit | edit source]Wrist
[edit | edit source]Joint Contact
[edit | edit source]Axis of Rotation
[edit | edit source]Hand
[edit | edit source]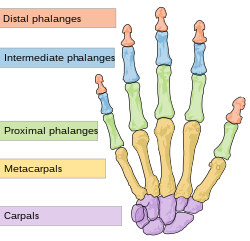

Table Radius of Curvature of the Middle Sections of the Metacarpal Head and Proximal Phalanx Base
| MCH index | Long | PPB index | Long | |
|---|---|---|---|---|
| Bony contour(Radius) | 6.42 ± 1.23 | 6.44 ± 1.08 | 13.01 ± 4.09 | 11.46 ± 2.30 |
| Cartilage contour(Radius) | 6.91 ± 1.03 | 6.66 ± 1.18 | 12.07 ± 3.29 | 11.02 ± 2.48 |
Source: Tamai K., Ryu J., An K.N., Linscheid R.L.,Cooney W.P., and Chao E.Y.S. 1988. J. Hand Surg.13A: 521.
Table Curvature of Carpometacarpal Joint Articular Surfaces
| n | Header text | Header text | Header text | Header text | |
|---|---|---|---|---|---|
| Trapezium | |||||
| Female | Example | Example | Example | Example | Example |
| Male | Example | Example | Example | Example | Example |
| Total | Example | Example | Example | Example | Example |
| Female vs. male | Example | Example | Example | Example | Example |
| Metacarpal | |||||
| Female | Example | Example | Example | Example | Example |
| Male | Example | Example | Example | Example | Example |
| Total | Example | Example | Example | Example | Example |
| Female vs. male | Example | Example | Example | Example | Example |
Note: Radius of curvature: ρ = 1/κ. Source: Athesian J.A., Rosenwasser M.P., and Mow V.C. 1992. J. Biomech. 25: 591.
Joint Contact
[edit | edit source]Axis of Rotation
[edit | edit source]Joint Lubrication
[edit | edit source]Tribology
[edit | edit source]Tribology comes from the Greek word, “tribos”,meaning “rubbing” or “to rub” and from the suffix, “ology” means “the study of”. Tribology is the study of rubbing, or... “the study of things that rub”. Tribology is a branch of mechanical engineering and materials science. This includes the fields of: friction, lubrication, and wear. It was coined by the British physicist David Tabor and also by Peter Jost in 1964 and started the new discipline of tribology.[5] Tribology is all around us as the follows:
| content | Examples |
|---|---|
| Individual components | Brake,clutch pads,gears,bearings and so on. |
| Assemblies or products | Engines,pocket watch,rock climbing shoes and so on. |
| Manufacturing processes | Rolling, turning, stamping, grinding, polishing and so on. |
| Construction/exploration | Mine slurry pumps,space shuttle, excavator,oil drilling rig, chunnel digging drill and so on. |
| Natural phenomena | On/off stiction:gecko feet, water and wind erosion, plate tectonics and so on. |
Surfaces in Contact
[edit | edit source]Every application has surfaces in contact in relative motion such as sliding, rolling and impacting. The surface is not simple and not flat. All engineering surfaces have a roughness, and this roughness has an important role in tribology. Surface roughness comes from all prior history of the part like manufacturing, handling and prior use in application.
Friction
[edit | edit source]

Friction is the resistant force to relative motion between solid surfaces, fluid layers, and material elements sliding against each other.
Static friction occurs when two or more solid objects are not moving relative to each other(like a desk on the ground). The coefficient of static friction, typically denoted as μs, is usually higher than the coefficient of kinetic friction.
Kinetic (or dynamic) friction is friction between two objects are moving relative to each other and rub together (like a sled on the ground). The coefficient of kinetic friction is typically denoted as μk, and is usually less than the coefficient of static friction for the same materials[6].
Rolling friction occurs when two objects move relative to each other and one "rolls" on the other (like a car's wheels on the ground). This is classified as one of static friction as the patch of the tire in contact with the ground, at any point while the tire spins, is stationary relative to the ground.
Fluid friction describes the friction between a solid object as it moves through a liquid or gas medium. The drag of air on an airplane, or that of water on a swimmer, are two examples of fluid friction. This internal resistance to flow is expressed as viscosity. Viscosity is measured with various viscometers and rheometers.
Lubrication
[edit | edit source]Lubrication is the process, or technique employed in order to reduce friction, to prevent wear, to transport debris away from interface and to provide cooling by interposing a substance called lubricant between the surfaces to carry or to help carry the load (pressure generated) between the surfaces. The types of lubrication may be classified according to the ratio of the squeeze film (oil film) thickness h and the surface roughness. But, full-film lubrication can be broken down into two forms: hydrodynamic and elastohydrodynamic.
- Hydrodynamic lubrication(h>Ra): It is also called fluid-film, thick-film, or flooded lubrication. The load is taken completely by the thick oil film. Hydrodynamic lubrication relies on the relative speed between the surfaces, oil viscosity, load, and clearance between the moving or sliding surfaces. Hydrodynamic lubrication is used to delicate instruments,light machines like watches, clocks, guns, sewing machines,scientific instruments, large plain bearings like pedestal bearings, main bearing of diesel engines.The Reynolds equations can be used to describe the principles for the fluids.And when gases are used, their derivation is much more involved.
- Elastohydrodynamic lubrication(h>Ra):The film elastically deforms the rolling surface to lubricate it.
- Transition from hydrodynamic and elastohydrodynamic lubrication to boundary lubrication(h~Ra):The lubrication goes from the desirable hydrodynamic condition of no contact to the less acceptable “boundary” condition, where increased contact usually leads to higher friction and wear. This regime is sometimes called as mixed lubrication.
- Boundary lubrication(also called boundary film lubrication) (h<Ra): The bodies come into closer contact at their asperities.Boundary lubrication occurs when a shaft starts moving from rest,the speed is very low,the load is very high and viscosity of the lubricant is too low.factors become important in the transition from hydrodynamic to boundary lubrication. The most important factor in boundary lubrication is the chemistry of the tribological system — the contacting solids and total environment including lubricants.
In hydrodynamic lubrication, the general Reynolds equation is:
Where:
- is fluid film pressure.
- and are the bearing width and length coordinates.
- is fluid film thickness coordinate.
- is fluid film thickness.
- is fluid viscosity.
- is fluid density.
- are the bounding body velocities in respectively.
- are subscripts denoting the top and bottom bounding bodies respectively.
The equation can either be used with consistent units or nondimensionalized. The Reynolds Equation assumes:
- The fluid is Newtonian.
- Fluid viscous forces dominate over fluid inertia forces. This is the principal of the Reynolds number.
- Fluid body forces are negligible.
- The variation of pressure across the fluid film is very small (i.e. )
- The fluid film thickness is much less than the width and length and thus curvature effects are negligible. (i.e. and )
Wear
[edit | edit source]Wear is erosion or sideways displacement(or removal) of material from one body when subjected to contact and relative motion with another body. Wear is about interactions between surfaces and more specifically the removal and deformation of material on a surface as a result of mechanical action of the opposite surface.[7] The requirement for relative motion between two surfaces and initial mechanical contact between asperities is an important difference between mechanical wear compared to other processes with similar results.[8]. Under normal mechanical and practical process, the wear-rate normally changes through three stages[9]
- Primary stage or early run-in period : surfaces adapt to each other and the wear-rate might be various(high or low).
- Secondary stage or mid-age process: a steady rate of ageing is in motion. Most of the components operational life is comprised in this stage.
- Tertiary stage or old-age period: the components fail rapidly due to a high rate of ageing.
Some commonly referred to wear mechanisms (or processes) contain:
- Abrasive Wear, Scratching :Abrasive wear occurs when a hard rough surface scratches a softer surface.[7]
- Adhesive Wear, Galling, Scuffing:Adhesive wear can be found between surfaces during frictional contact and generally means unwanted displacement and attachment of wear debris and material compounds from one surface to another. Adhesive wear starts as “local welding”. Material “compatibility” is important for adhesive wear. Stacking fault energy,crystal structure, natural oxide formation all have an impact on adhesive wear.
- Fretting/Fretting Corrosion:
- Erosive Wear, Cavitation, Impact, Electro-arcing
- Rolling Contact Fatigue, Spalling, Delamination:Fatigue is a process the surface of a material is weakened by the loading. Reversing sub-surface shear each time the roller or ball passes over the surface. Accumulation of these stresses cause subsurface crack formation, usually at a microstructural inhomogeneity. Debris usually gets rolled over,creating additional damage. Cracks grow toward surface and particle spalls off.
- Tribo-Corrosion
These wear mechanisms do not act independently and wear mechanisms are not mutually exclusive.[8]
Biotribology
[edit | edit source]
Biotribology has been one of the most active topics in tribology during the past 40 years. Biotribology can be expressed as the study of friction, wear and lubrication of biological systems, mainly synovial joints such as the human hip and knee.
Synovial fluid
[edit | edit source]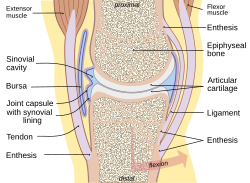
Synovial fluid is a viscous, non-Newtonian fluid in the cavities of synovial joints. With its yolk-like consistency ("synovial" partially derives from ovum, Latin for egg), synovial fluid reduce friction between the articular cartilage of synovial joints during movement. Between shocks, the synovial fluid in diarthrotic joints becomes thick to protect the joint and then thins to normal viscosity. The fluid provides oxygen and nutrients and removes carbon dioxide and metabolic wastes from the chondrocytes within the surrounding cartilage.
The normal volume of synovial fluid obviously varies from joint to joint. Normal synovial fluid contains 3–4 mg/ml hyaluronan (hyaluronic acid). [10] Hyaluronan is synthesized by the synovial membrane and secreted into the joint cavity to increase the viscosity and elasticity of articular cartilages and to lubricate the surfaces between synovium and cartilage.[11] Synovial fluid includes lubricin (also known as PRG4) as a second lubricating component, secreted by synovial fibroblasts.[12] It has an essential role in so-called boundary-layer lubrication, which reduces friction between the surface of cartilage. In addition, it helps regulate synovial cell growth.[13] It also includes phagocytic cells that remove microbes and the debris that results from normal wear and tear in the joint. And it is related to the change of pH in the synovial fluid.[14]
Joint Lubrication
[edit | edit source]Glucosamine
[edit | edit source]
Glucosamine(C6H13NO5) is an important component of cartilage, mucous membranes, and synovial fluid. It can be manufactured in the lab or extracted from the exoskeletons of lobsters, crabs, shrimp, and other sea creatures. It can be found in various forms like glucosamine sulfate,glucosamine hydrochloride and n-acetyl glucosamine. Efficacy of glucosamine is generally considered to be good and is supported by several studies.In the United States, glucosamine is not approved by the Food and Drug Administration for medical use in humans.[15] Since glucosamine is categorized as a dietary supplement in the US, safety and formulation are solely the responsibility of the manufacturer[16] . In most of Europe, glucosamine is approved as a medical drug and is sold in the form of glucosamine sulfate.[17]
Major side effects of all glucosamine salt are mild gastrointestinal problem such as constipation, diarrhea, cramping, gas, heartburn, and nausea. Glucosamine sulfate has been related to drowsiness and headache. The effects of glucosamine on nursing or pregnant women have not been studied well[18]. As glucosamine is an amino sugar and a prominent precursor for glucosaminoglycans, it may increase blood sugar levels. As glucosamine is often made from shellfish and the source of the product does not need the label, people who are allergic to seafood are advised to exercise caution as well.
Chondroitin
[edit | edit source]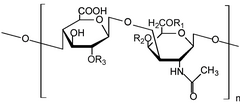
Like glucosamine, chondroitin is another major component of cartilage. Chondroitin can be manufactured synthetically, but is usually extracted from cow and shark cartilage. Chondroitin is in dietary supplements used as an substitutive medicine to treat osteoarthritis and also approved and regulated as a symptomatic slow-acting drug for this disease (SYSADOA) in Europe and some other countries.[19] It is commonly sold together with glucosamine. Chondroitin and glucosamine are used in veterinary medicine,too.[20]
Major side effects of chondroitin are uncommon but contains hair loss and minor gastrointestinal complaints. The effects of chondroitin on nursing or pregnant women have not been studied well. Chondroitin can decrease the blood’s ability to clot, and it is not good to take it with aspirin, antiplatelet, or anticoagulant drugs. As glucosamine and chondroitin are both components of cartilage, they are sometimes combined in one product. Chondroitin products are also sometimes combined with manganese, which may help cartilage production, but is toxic in large doses. The U.S. National Academy of Sciences has set the adult tolerable upper limit for manganese at 11 mg/day; patients should be advised not to overdose that level[21][22].
MSM(Methylsulfonylmethane)
[edit | edit source]
Methylsulfonylmethane (MSM) is an organosulfur compound with the chemical formula (CH3)2SO2. It is also known as DMSO2, methyl sulfone, and dimethyl sulfone.[23] MSM is sold as a dietary supplement and often combined with glucosamineand/or chondroitin sulfatefor helping to treat or prevent osteoarthritis. According to one review, "The benefits claimed for MSM far exceed the number of scientific studies. It is hard to build a strong case for its use other than for treating arthritis problems."[24] In 1978, the FDA approved DMSO for instillation into the bladder as a treatment for interstitial cystitis. Since DMSO is metabolized to MSM by the body, MSM could be the active ingredient in DMSO treatments.[25] In October 2000, the United States FDA warned one MSM promoter, Karl Loren, to cease from making therapeutic claims for MSM.[26]
Omega-3 fatty acid
[edit | edit source]
Omega-3 fatty acids (also called n-3 fatty acids or ω-3 fatty acids)[27]) are polyunsaturated fatty acids with a double bond(C=C) at the third carbon atom from the end of the carbon chain.[28] The fatty acids have two ends, the carboxylic acid end, which is the beginning of the chain, thus "alpha", and the methyl end, which is the "tail" of the chain, thus "omega." The nomenclature of the fatty acid is from the location of the first double bond, counted from the methyl end, that is, the omega (ω-) or the n- end. The three types of omega-3 fatty acids related to human physiology are α-Linolenic acid(ALA, which is plantiful in plant oils), Eicosapentaenoic acid(EPA), and Docosahexaenoic acid(DHA) (both commonly found in fish oils).
Hyaluronic acid
[edit | edit source]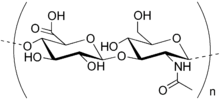
Hyaluronan is an anionic, nonsulfated glycosaminoglycan which exist in connective, epithelial, and neural tissues. It is unique and can be very large, with its high molecular weight often close to the millions.[29] In the extracellular matrix, hyaluronan has a essential role in cell proliferation and migration, and may also be involved in the progression of some malignant tumors.[30]. Hyaluronic acid as a component synovial fluid is commonly injected into the joint as a treatment for osteoarthritis. It has not been proven to generate benefit and has potential side effects.[31] In 2007, the European Medicines Agency extended its approval of Hylan GF-20 as a treatment for ankle and shoulder osteoarthritis pain.[32]
Several manufacturers have begun producing oral versions, but clinical evidence for efficacy of oral hyaluronic acid in the treatment of arthritis is not clear.
Shark cartilage
[edit | edit source]Shark cartilage is a dietary supplement from the dried and powdered cartilage of a shark. It is the tough material that composes a shark's skeleton. There is no scientific evidence that shark cartilage is good for treating or preventing cancer or other diseases.[33] But,it has also been promoted as a treatment for both rheumatoid arthritis and osteoarthritis[34]. No studies have been proceeded to find out whether shark cartilage has any side effects.
Hydrogel Artificial Cartilage
[edit | edit source]
As candidate material of artificial cartilage, PVA( poly(vinyl alcohol)) hydrogel showed excellent lubricity and enhancement of fluid film formation compared to UHMWPE(ultra high molecular weight polyethylene)[35].In addition, Poly(vinyl alcohol) (PVA) hydrogel has excellent biocompatibility and mechanical properties[36][37]. Polyvinyl alcohol (PVOH, PVA, or PVAl) is a watersoluble synthetic polymer. It has the idealized formula [CH2CH(OH)]n. PVA is prepared by first polymerization of vinyl acetate, and the resulting polyvinylacetate is converted to the PVA.[37] It has high tensile strength and flexibility including high oxygen and aroma barrier properties. However these properties can be controlled by humidity. The water will then reduce its tensile strength, but increase its elongation and tear strength. PVA has a melting point of 230 °C and 180–190°C (356-374 degrees Fahrenheit) for the fully hydrolysed and partially hydrolysed grades, respectively. It decomposes rapidly above 200 °C as it can undergo pyrolysis at high temperatures. The Poisson's ratio is between 0.42 and 0.48.[38]
Joint Lubrication Development
[edit | edit source]Gait Analysis
[edit | edit source]
Gait analysis is a method used to assess the way we walk or run to highlight biomechanical abnormalities such as overpronation, oversupination, increased Q angle, hip hiking (or hitching),ankle equinus, pelvic tilt. Gait analysis is usually performed by a professional like a podiatrist or physiotherapist. But it becomes popular and easily available with many specialist running and sports shops[39].
Further Reading
[edit | edit source]- Bronzino, Joseph D. (April 2006). The Biomedical Engineering Handbook, Third Edition. [CRC Press]. ISBN 978-0-8493-2124-5.
- Villafane, Carlos, CBET. (June 2009). Biomed: From the Student's Perspective, First Edition. [Techniciansfriend.com]. ISBN 978-1-61539-663-4.
{{cite book}}: CS1 maint: multiple names: authors list (link) - Information related to biomedical engineering.
Practise
[edit | edit source]Reference
[edit | edit source]- ↑ Ankle at eMedicine Dictionary
- ↑ Brent K. Milner, Ryan S. Fajardo (2007) Musculoskeletal Imaging, in Spencer B. Gay (editor) Radiology Recall p.294
- ↑ James G. Adams, Erik D. Barton, Jamie Collings (2008) Emergency Medicine: Expert Consult p.2660
- ↑ Scott J, Lee H, Barsoum W, van den Bogert AJ (November 2007). "The effect of tibiofemoral loading on proximal tibiofibular joint motion". J. Anat. 211 (5): 647–53. doi:10.1111/j.1469-7580.2007.00803.x. PMC 2375777. PMID 17764523.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Mitchell, Luke (November 2012). Ward, Jacob (ed.). "The Fiction of Nonfriction". Popular Science. No. 5. 281 (November 2012): 40.
{{cite journal}}:|access-date=requires|url=(help) - ↑ Sheppard, Sheri; Tongue, Benson H. and Anagnos, Thalia (2005). Statics: Analysis and Design of Systems in Equilibrium. Wiley and Sons. p. 618. ISBN 0-471-37299-4. "In general, for given contacting surfaces, μk < μs"
- ↑ a b Rabinowicz, E. (1995). Friction and Wear of Materials. New York, John Wiley and Sons.
- ↑ a b Williams, J. A. (2005). "Wear and wear particles - Some fundamentals." Tribology International 38(10): 863-870
- ↑ Chattopadhyay, R. (2001). Surface Wear - Analysis, Treatment, and Prevention. OH, USA: ASM-International. ISBN 0-87170-702-0.
- ↑ Hui, Alexander Y.; McCart, William J.; Masuda, Koichi; Firestein, Gary S.; Sah, Robert L. (Jan–Feb 2012). "A Systems Biology Approach to Synovial Joint Lubrication in Health, Injury, and Disease". Systems Biology and Medicine. Wiley Interdisciplinary Reviews. 4 (1): 15–7. doi:10.1002/wsbm.157. PMC 3593048. PMID 21826801.
- ↑ "Joints". University of Washington Medicine - Department of Orthopaedics and Sports Medicine. Retrieved 2013-02-04.
- ↑ Jay, GD; Britt, DE; Cha, CJ (March 2000). "Lubricin is a product of megakaryocyte stimulating factor gene expression by human synovial fibroblasts". J Rheumatol (abstract). 27 (3): 594–600. PMID 10743795.
{{cite journal}}:|access-date=requires|url=(help) - ↑ Warman M (2003). "Delineating biologic pathways involved in skeletal growth and homeostasis through the study of rare Mendelian diseases that affect bones and joints". Arthritis Research & Therapy. 5 (Suppl 3): S2. doi:10.1186/ar804.
- ↑ Ward TT, Steigbigel RT: Acidosis of synovial fluid correlates with synovial fluid leukocytosis. Am .I Med 64:933, 1978
- ↑ Hubbard WK, Associate Commissioner of Policy and Planning (2004; update 2012). "Letter Regarding the Relationship Between the Consumption of Glucosamine and/or Chondroitin Sulfate and a Reduced Risk of: Osteoarthritis; Osteoarthritis-related Joint Pain, Joint Tenderness, and Joint Swelling; Joint Degeneration; and Cartilage Deterioration(Docket No. 2004P-0059)". United States Department of Health and Human Services, Food and Drug Administration. Retrieved 14 May 2014.
{{cite web}}:|author=has generic name (help); Check date values in:|year=(help) - ↑ "Complementary and Alternative Medicine Use Among Adults and Children: United States, 2007" (PDF). National Center for Health Statistics. December 10, 2008. Retrieved 2009-08-16.
- ↑ Jordan KM; Arden NK; Doherty M; et al. (December 2003). "EULAR Recommendations 2003: a evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT)". Annals of the Rheumatic Diseases. 62 (12): 1145–55. doi:10.1136/ard.2003.011742. PMC 1754382. PMID 14644851.
{{cite journal}}:|first10=missing|last10=(help);|first11=missing|last11=(help); Unknown parameter|author-separator=ignored (help) - ↑ Letic-Gavrilovic A, Scandurra R, Abe K. Genetic potential of interfacial guided osteogenesis in implant devices. Dent Mater J. Jun 2000;19(2):99-132.
- ↑ Jordan KM, Recommendations Arden NK. EULAR (2003). "an evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT)". Ann Rheum Dis. 62 (12): 1145–1155. doi:10.1136/ard.2003.011742. PMC 1754382. PMID 14644851.
- ↑ Forsyth R, Brigden C, Northrop A (2006). "Double blind investigation of the effects of oral supplementation of combined glucosamine hydrochloride (GHCL) and chondroitin sulfate (CS) on stride characteristics of veteran horses". Equine veterinary journal. Supplement. 38 (36): 622–5. doi:10.1111/j.2042-3306.2006.tb05615.x. PMID 17402494.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Letic-Gavrilovic A, Scandurra R, Abe K. Genetic potential of interfacial guided osteogenesis in implant devices. Dent Mater J. Jun 2000;19(2):99-132.
- ↑ Drug Digest
- ↑ "Various Names for MSM" (PDF). Retrieved June 8, 2009.
- ↑ "Pharmacists review the effectiveness, benefits and side effects of MSM".
- ↑ Childs, SJ (1994). "Dimethyl sulfone (DMSO2) in the treatment of interstitial cystitis". The Urologic clinics of North America. 21 (1): 85–8. PMID 8284850.
- ↑ Warning letter to Karl Loren, Vibrant Life/B&B International", FDA Center for Food Safety and Applied Nutrition, 20 October 2000
- ↑ "Related terms". Omega-3 fatty acids, fish oil, alpha-linolenic acid. Mayo Clinic. Retrieved June 20, 2012.
- ↑ Scorletti, E; Byrne, CD (2013). "Omega-3 fatty acids, hepatic lipid metabolism, and nonalcoholic fatty liver disease". Annual review of nutrition. 33: 231–48. doi:10.1146/annurev-nutr-071812-161230. PMID 23862644.
- ↑ Fraser, J.R.E; Laurent, T. C.; Laurent, U. B. G.; et al. (1997). "Hyaluronan: its nature, distribution, functions and turnover" (PDF). Journal of Internal Medicine. 242 (1): 27–33. doi:10.1046/j.1365-2796.1997.00170.x. PMID 9260563. Retrieved 2009-06-05.
{{cite journal}}: Explicit use of et al. in:|first=(help) - ↑ Stern, edited by Robert (2009). Hyaluronan in cancer biology (1st ed. ed.). San Diego, CA: Academic Press/Elsevier. ISBN 978-0-12-374178-3.
{{cite book}}:|edition=has extra text (help);|first=has generic name (help) - ↑ Rutjes, AW (Aug 7, 2012). "Viscosupplementation for osteoarthritis of the knee: a systematic review and meta-analysis". Annals of internal medicine. 157 (3): 180–91. doi:10.7326/0003-4819-157-3-201208070-00473. PMID 22868835.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ↑ "Hylan G-F 20 (Synvisc) approved by EMEA for pain due to ankle and shoulder OA". National Health Service. Retrieved 2007-07-09.
- ↑ "Shark Cartilage". American Cancer Society. November 1, 2008.
- ↑ "Efficacy and tolerability of chondroitin sulfate 1200 mg/day vs chondroitin sulfate 3 x 400 mg/day vs placebo". US National Library of Medicine, National Institutes of Health. May 6, 1998.
- ↑ Kazuhiro Nakashima, Yoshinori Sawae, Nobuaki Tsukamoto, Hiromasa Miura, Yukihide Iwamoto,Teruo Murakami,Wear Behaviour of an Artificial Cartilage Material for Hemiarthroplasty,6th World Congress of Biomechanics (WCB 2010). August 1-6, 2010 Singapore IFMBE Proceedings Volume 31, 2010, pp 1169-1172
- ↑ Sheng Wu Yi Xue Gong Cheng Xue Za Zhi. Review of poly(vinyl alcohol) hydrogel and its compounds in the application of artificial cart,2003 Dec;20(4):742-5.
- ↑ a b Manfred L. Hallensleben "Polyvinyl Compounds, Others" in Ullmann's Encyclopedia of Industrial Chemistry, 2000, Wiley-VCH, Weinheim. Template:DOI
- ↑ Characterization of PVA cryogel for intravascular ultrasound elasticity imaging, Fromageau, J.; Brusseau, E.; Vray, D.; Gimenez, G.; Delachartre, P.; IEEE Transactions on Ultrasonics, Ferroelectrics and Frequency Control, Volume: 50, Issue: 10. 2003, Page(s): 1318 - 1324.
- ↑ Levine DF, Richards J, Whittle M. (2012). Whittle's Gait Analysis Whittle's Gait Analysis Elsevier Health Sciences. ISBN 978-0702042652

















