A-level Biology/Central Concepts/Control, coordination and homeostasis
Homeostasis
[edit | edit source]Homeostasis is the internal maintenance of a stable internal environment - temperature, amount of water and amount of glucose. If temperature is too high, the enzymes could become denatured. Too low, and metabolic processes will be too slow. Lack of water causes water to be drawn out via osmosis causing metabolic reactions to stop, whereas too much water will cause the cell to burst. Lack of glucose causes respiration to stop, whilst too much glucose may draw water out of the cell via osmosis.
Homeostasis is achieved using a negative feedback control loop, involving a receptor and an effector. The receptor receives information about the parameter being regulated, the input, and sets off a series of events culminating in an action by the effector, the output. Continuous monitoring keeps the parameter around an ideal level, and in negative feedback a rise in the parameter results in something happening that makes the parameter fall.
A positive feedback system is a problem - for example in high carbon dioxide concentration air, a person breathing will have high carbon dioxide concentrations in the blood, causing the carbon dioxide receptors to increase the breathing rate, breathing in more carbon dioxide.
Excretion
[edit | edit source]The removal of unwanted products of metabolism is called excretion. The two biggest excretory products in humans are urea and carbon dioxide. Urea is produced by the liver from excess amino acids and is transported from the liver to the kidneys in the blood, and the kidneys remove urea and excrete it dissolved in water, as urine. Urea is the main nitrogenous excretory product of humans.
Carbon dioxide is produced in every cell in the body, as a product of aerobic respiration, and is transported in the bloodstream to the lungs and is exhaled.
Deamination
[edit | edit source]The body must get rid of nitrogenous wastes from nucleic acids and proteins. The protein that we do not use is converted to urea, with the liver salvaging the energy by removing the nitrogen atoms, and this process is known as deamination. The amino group of an amino acid is removed with an extra hydrogen atom, and combines to produce ammonia, a soluble and highly toxic compound. Because of ammonia's toxicity, this ammonia is rapidly converted to the less soluble and less toxic compound, urea.
Kidney structure
[edit | edit source]

The human body has two kidneys, and each receives blood via a renal artery and returns blood via a renal vein. The ureter carries urine from the kidney to the bladder, which excretes urine to the outside of the body via the urethra. The picture to the right shows a longitudinal section through a kidney, and it's clear that the kidney is covered by a tough capsule, beneath which is the cortex. The central area is the medulla, and where the ureter joins there is an area known as the pelvis. A microscope section shows that the kidney is made up of thousands of tubes known as nephrons.
The nephrons structure is shown in the second picture down, and the labelled glomeluar capsule is known also as a renal or Bowman's capsule, and the renal capsules of all nephrons are in the cortex. They then run towards the centre of the kidney, forming a twisted region called the proximal convoluted tubule (PCT), and then a long loop of Henle (in the medulla). This then runs back up toward to cortex where it forms another twisted region called the distal convoluted tubule, before reaching a collecting duct which leads down through the medulla and into the pelvis of the kidney, joining the ureter.
The linked picture shows the distribution of blood vessels in cortex of kidney, including how each renal capsule is supplied with blood from a branch of the renal artery known as an afferent arteriole that leads to the glomerulus, a tangle of capillaries in the capsule. These capillaries then rejoin to form an efferent arteriole that leaves the capsule to rejoin with the vein.
Ultrafiltration
[edit | edit source]Urine production is a two-part process, ultrafiltration and reabsorption. The former is done in the renal capsule, where small molecules, including urea are taken out of the blood and into the renal capsule where they take the nephrons route through the kidney.
Structure of a renal capsule is as follows;
- Network of capillaries that come from the afferent arteriole, separated by two cell layers from the renal capsule lumen.
- The first cell layer is endothelium cells, with thousands of tiny gaps.
- The second cell layer is the basement membrane formed from epithelial cells which make up the wall of the renal capsule, and have many finger-like projections, and have gaps. They are known as podocytes.
- The holes in the capillary endothelium and renal epithelium are large enough to allow any dissolved substances in the blood to get through. The basement membrane stops large protein molecules from getting through, as well as blood cells.
The rate of ultafiltration is known as the glomerular filtration rate, and is usually around 125 cm3min−1. This is due to a variety of factors. The concentration of solutes in the blood plasma in the capillaries is higher than in the renal capsule, since the plasma protein molecules are too big to get through, creating a water potential that is lower in the blood capillaries.
However, the water potential of the blood plasma is raised by the pressure inside the capillaries, causing blood to continue to move down this water potential gradient from the blood to the capsule.
Reabsorption
[edit | edit source]Many of the filtered substances need to be kept in the body, and so are selectively reabsorbed (as some of them do need to be excreted). Most of this process occurs in the proximal convoluted tubule, when a large part of the filtrate is reabsorbed back into the blood in the capillary netwrok.
The mechanisms of reabsorption are: 1- Active transport of glucose and amino acids. 2- Active transport and facilitated diffusion of mineral ions. 3- Movement of water by osmosis.
Proximal Convoluted Tubule
[edit | edit source]Na+/-K+ pump in proximal tubule cell membrane using ATP (made by its numerous mitochondria) to transport sodium ions out of the cell into the blood plasma, lowering the concentration inside the cell, so that they can passively diffuse (using the created concentration gradient) back into it from the proximal tubule. The sodium ions use special transporter proteins, at the same time taking up glucose from the proximal tube and is then taken into the blood. The membrane itself is folded to increases surface area for exchange on the blood plasma side.
Glucose, amino acids, vitamins, 65% of the water from the PCT and many sodium/chloride ions are actively reabsorbed here. Some urea is also reabsorbed, around half. The numerous microvilli on the proximal tubule side provide an increased surface area for uptake of solutes. This reduces the volume of liquid remaining from 125 cm3 to around 45 cm3 to go to the loop of Henle.
Loop of Henle
[edit | edit source]The loop of Henle serves to create a high concentration of salts in the tissue fluid in the medulla of the kidney, allowing a lot of water to be reabsorbed from the fluid in the collecting duct as it flows through, producing very concentrated urine and preserving water for the body.
As you can see in the above picture, there is a descending and ascending limb. The method by which it concentrates urine is below;
- 1. Sodium and Chloride are actively transported out of the ascending limb
- 2. This raises the concentration of sodium and chloride in the tissue fluid
- 3. This in turn causes loss of water into the tissue fluid in the descending limb.
- 4. This loss of water concentrates sodium and chloride in the descending limb
- 5. The concentrated sodium and chloride ions can then diffuse out of the ascending limb into the tissues.
Having the two limbs run side by side allows maximum concentration to be built up both inside and outside the tube at the bottom, and is known as a counter-current multiplier.
The fluid then is flowing up the ascending limb of the loop of Henle, losing sodium and chloride as it goes, it continues round into the collecting duct, which dips into the medulla again, passing through the high-solute concentration regions of the tissues. This causes yet more water to move out of the collecting duct via osmosis.
Distal Convoluted Tubule
[edit | edit source]The first part of the DCT acts in the same way as the ascending loop of Henle, the second part behaves in the same way as the collecting duct. Functions of second part of the DCT and collecting duct are below;
- Sodium ions are actively pumped from the fluid in the tubule into the tissue fluid, where they pass into the blood.
- Potassium ions are actively transported into the tubule
Osmoregulation
[edit | edit source]The control of water in an organism is known as osmoregulation.
Hypothalamus
[edit | edit source]Osmoreceptors within the hypothalamus detect when the water potential in the blood is low since the loss of water reduces their volume which triggers stimulation of nerve cells in the hypothalamus. The hypothalamus are receptors and the effector is the pituitary gland and the walls of the distal convoluted tubule. The stimulated nerve cells produce a chemical known as antidiuretic hormone (ADH), a poly peptide made up of nine amino acids. When nerve cells are stimulated by the osmoreceptors, action potentials travel down them, causing ADH to be released from the blood in the capillaries in the posterior pituitary gland.
ADH
[edit | edit source]Antidiuretic hormone, or ADH is a hormone that is produced in the hypothalamus and stored and released in the pituitary gland. It acts on the kidney cells making up the walls of the collecting ducts, increasing their permeability to water by increasing the amount of water channels in the plasma membrane. ADH makes the blood more dilute by increasing the concentration of the urine. This is used to control the saltiness of the urine. If an organism does not have enough water, ADH will be activated to increase reabsorption of water.
Negative feedback
[edit | edit source]Again this is a negative feedback system - when blood water content is low, the hypothalamus acts to make the pituitary gland release ADH, and stops once blood water content rises (since the osmoreceptors are no longer being stimulated).
Hormones
[edit | edit source]Exocrine/Endocrine
[edit | edit source]An endocrine gland is one that secretes hormones directly into the blood. Exocrine glands are glands that secrete to the outside, into a tube or a duct along which the secretion flows.
Structure/Function of Hormones
[edit | edit source]Structure:
- Relatively small
- Can be proteins or steroids
- Usually have a short life in the body and are broken down by enzymes, or lost in urine.
- Secreted in a very small concentration
Function:
- To carry information from one part of a mammals body to another part
- Respond to stimulus (such as adrenaline responding to a frightening stimulus)
- Transported by the blood and have a group of cells which it affects - target cells. These target cells contain receptors specific to the hormone.
Pancreas
[edit | edit source]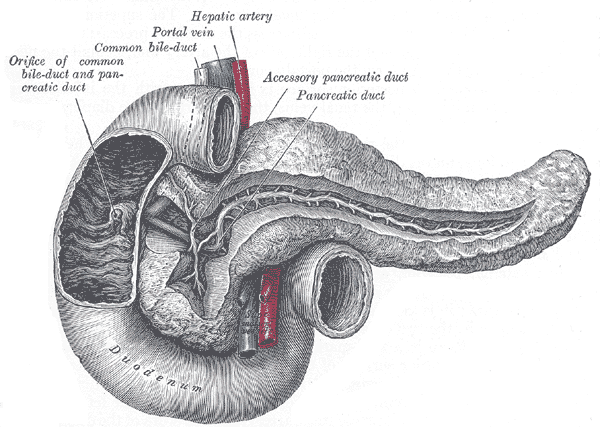
The picture on the right shows the structure of the pancreas. The pancreas is unique in that it is both an exocrine and an endocrine gland - separate parts taking care of each. The exocrine function is the secretion of pancreatic juice which flows along the pancreatic duct into the duodenum. The endocrine function is the secretion of glucagon and insulin, by the α and β cells, respectively, of the islets of Langerhans.
Blood glucose
[edit | edit source]Blood glucose levels are controlled by the secretion of glucagon and insulin by the islets of langerhans. When the stomach has carbohydrates in it, glucose from the digested food is absorbed from the small intestine and passed into the blood. When this blood flows through the pancreas, the α and β cells detect the raised glucose levels. α cells respond by stopping the secretion of glucagon (glucagon converts glycogen (a storage molecule) to glucose, it also produces glucose from other compounds and uses fatty acids instead of glucose as the main fuel in respiration.), whilst β cells secrete insulin into the blood plasma, where it is carried to all parts of the body.
Insulin acts to lower blood glucose by the following methods;
- Increase in the rate of use of glucose in respiration
- Increased absorption of glucose into cells
- Increase at the rate at which glucose is converted into glycogen
Once blood glucose levels are back to normal, α cells start secreting glucagon again and β cells stop secreting insulin. It is a continuous cycle - with glucagon raising the glucose levels, insulin may have to be switched on again soon - and blood sugar levels never remain constant because of the time delay between a change and a correction.
Diabetes mellitus
[edit | edit source]There are two forms of diabetes;
- Insulin-dependent diabetes - this is when the pancreas cannot secrete enough insulin, and requires regular insulin injections.
- Non-insulin-dependent diabetes - This is when the pancreas does secrete insulin but neither the liver or muscle cells respond properly to it, and usually begins relatively late in life and is associated with obesity.
Symptoms for both are the same;
- After a carbohydrate meal, blood glucose levels rise and stay high
- Glucose can appear in the urine, along with extra water and salts, causing the person to feel hungry and thirsty constantly
Suggested reading: Insulin
Control of insulin secretion
[edit | edit source]β cells in the islets of Langerhans release insulin in response to the high levels of glucose in the blood. They do this via the following functions
- 1. K+ (Potassium) channels in the plasma membrane are open, K+ diffuses out and the inside of the cell is -70mV compared to outside (potential difference)
- 2. Glucose enters the cell if there are high glucose levels
- 3. Glucose is phosphorylated by the enzyme glucokinase and metabolised to produce ATP.
- 4. The presence of extra ATP makes K+ channels close
- 5. K+ cannot diffuse out, and the potential difference reduces to around -30mV
- 6. Ca2+ channels that are usually close open in response to the change in membrane potential.
- 7. Ca2+ ions cause the vesicles (created by the golgi apparatus, full of insulin) to release insulin by exocytosis
Nervous communication
[edit | edit source]
Neurones
[edit | edit source]The other method (except hormones) is an electrical signal system along pathways, and the cells that make these paths and carry the signals are known as neurones. The picture to the right shows a motor neurone which transmits messages from the brain to a muscle or gland. The cell body of this neurone always lies within the spinal cord or brain. The dendrites (labelled) are processes and conduct impulses towards the cell body. The long process is known as an axon (labelled), and may stretch from the brain/spinal cord all the way to your foot, so can be extremely long. Large numbers of mitochondria are found at the terminal branches, with vesicles containing transmitter substances.
The Schwann cells (they are not in every neurone) wrap themselves round the axon all the way along, enclosing the axon in a myelin sheath, which affects the speed of conduction. The small uncovered areas of axon between Schwann cells are known as nodes of Ranvier, which together with the myelin sheath massively increase the speed of conduction.
A sensory neurone is similar to a motor neurone except it has one long dendron and is designed to bring impulses to the brain.
Reflex arc
[edit | edit source]A reflex arc is the pathway along which impulses are carried from a receptor to an effector, without conscious thought - reflexes. The impulse comes from the receptor, up the dorsal root of the spinal nerve, crosses into an intermediate neurone, and then reaches the cell body of motor neurone. It then immediately leaves to the effector via the ventral root of the spinal nerve. Also this transmission of the impulse does not include the assistance of the brain, only the spinal cord. The reflex arc is a fast response to a stimuli ,for instance the prickling of a finger by a sharp pin.
Transmission
[edit | edit source]Transmission of nerve impulses is controlled by rapid movememnt of sodium/potassium ions in/out of the axon, and not electrons such as in an electric current. In a resting axon, the inside has a slightly negative electrical potential when compared with the outside - this is known as the potential difference (usually -65mV). This resting potential is maintained by the sodium-potassium pump of the axon, which serves to carry sodium ions to the outside and potassium to the inside utilising active transport against their concentration gradients.
Action potentials
[edit | edit source]An action potential is the rapid fleeting change in potential difference across the membrane of an axon when an electric current is applied. This electric current controls voltage-gated channels for sodium and potassium in the axons plasma membrane. This is a two part process - first, the electric current stimulates the axon to open channels in the plasma membrane for sodium to come through, and they flood through, depolarising that section of the axon, until it reaches +40mV. At this point, sodium channels close and potassium channels open and potassium ions diffuse out of the axon down their concentration gradient, known as re polarisation. So many potassium ions flood out that there is a brief overshoot in negativity of the potential difference, but this is corrected by the sodium potassium pump - restoring the action potential
These action potentials are just for one area of the axon - how does information get taking along a neurone? The depolarisation of the membrane of any part of the axon sets up a 'local circuit' between the depolarised region and the resting regions either side - sodium ions flow sideways inside the axon towards the resting regions, depolarising them and setting off an action potential. The reason that information can be sent one way via a neurone (and does not keep coming back on itself) is that directly after an action potential, whilst the sodium-potassium pump is returning things to normal and cannot create a new action potential - the refractory period.
What starts it?
[edit | edit source]An action potential in an organism is started by a receptor cell, responding to stimulus. They convert one energy form to another, light, heat or sound into energy in an electrical impulse in a neurone. The receptor you are required to know about is the Pacinian corpuscle, a receptor found in the dermis of the skin. They contain an ending of a sensory neurone surrounded by a capsule.
When pressure is applied to a Pacinian corpuscle, the capsule is pressured out of shape, deforming the nerve ending inside, allowing sodium/potassium channels to open in the cell membrane, depolarising it. This increased positive charge inside the axon is called a receptor potential. The more pressure applied, the more channels open and the greater the receptor potential comes, and if it is over a certain threshold, it will be large enough to trigger an action potential. If not, it will remain as a local depolarization.
A simple A level definition of an action potential is a reverse of charge in resting potential caused by a moving impulse in the neurone.
Stimulus
[edit | edit source]The intensity of the stimulus does not increase the speed or 'power' of the action potential, since speed is always the same - what a strong stimulus does (and how it tells the brain that it is strong) is have a rapid succession of action potentials each one following just behind the other. Also, a strong stimulus is more likely to stimulate many neurones as opposed toa weak stimulus. So, the frequency of action potentials, number of neurones carrying action potentials give the brain information about the strength of the stimulus.
Speed
[edit | edit source]Axons with a myelin sheath can transmit nerve impulses around a 100 metres a second, whilst nonmyelinated neurones can only transmit at a speed of 0.5 metres a second. This is due to myelin insulating the axon membrane, and so sodium and potassium ions cannot flow through the myelin sheath and depolarise any area of the axon surrounded by it. So, in a myelinated neurone, it can only occur at the nodes of Ranvier. This is known as saltatory conduction, and action potentials jump from one node (of Ranvier) to the next, 1-3mm, and this can increase the transmission by up to 50x.
Diameter of axon also affects speed of transmission
Synapses
[edit | edit source]A synapse is where two neurones meet, and includes the parts of the two neurones next to each other and the small gap between them known as the synaptic cleft (cleft means gap).
Mechanism
[edit | edit source]Obviously from what you now know about action potentials, there is no way for them to jump like an electric current can. Instead, a transmitter substance is used, a chemical. An action potential travelling along a neurone reaches a the presynaptic neurone of a synapse, causes it to release it's transmitter substance which diffuses across the synaptic cleft to the postsynaptic membrane, setting up an action potential there and continuing the message.
More detail of this process is below;
- 1. An action potential arrives at the presynaptic membrane.
- 2. The action potential causes calcium channels to open, thus uptake of calcium ions.
- 3. The calcium ions cause vesicles containg acetylcholine (a transmitter substance) to fuse with the presynaptic membrane
- 4. Acetylcholine is then released and diffuses across the synaptic cleft.
- 5. The acetylcholine molecules then bind with the postsynaptic membranes receptors, opening sodium channels.
- 6. The sodium ions that consequently flood in depolarise the membrane and initiate an action potential.
- 7. Acetylcholine is hydrolysed and diffuses back across the synaptic into the presynaptic neurone.
To prevent acetylcholine keeping the sodium channels open, creating continuous action potentials, the synaptic cleft contains acetylcholinesterase, an enzyme that splits each Ach molecule into acetate and choline. The choline is then taken back to the presynaptic neurone, and combined with acetyl co-enzyme A to form ACh once more, and prepares in vesicles for the next action potential.
Neuromuscular junctions
[edit | edit source]This is between a motor neurone and a muscle where the nerve forms motor end plates, and the synapse is called the neuromuscular junction.
Roles
[edit | edit source]So why do we have synapses - they slow down a stimulus response since they break up the route.
- Synapses increase the range of reactions in response to a stimulus - the action potentials created by neurones come together at synapses, and your reaction can be determined by this - if you have to decide whether to pull out at a junction for example, action potentials from your eyes and ears telling your brain there is a car coming will make it more difficult for the action potentials from your brain thinking 'I'm late'. Action potentials from your eyes and ears outweigh. However, reflex reactions are quick and automatic, and the value of a rapid response is greater than a considered one if it saves your life.
- Synapses are involved in memory and learning.
- Synapses ensure one-way transmission, allowing signals to be directed and not spread at random.
note: Synapses travel in one direction because only the presynaptic neurone has vesicles containing neurotransmitter
Receptors are found on the postsynaptic neurone
- Summation.( low frequency impulses that produce insufficient amounts of neurotransmitter to trigger a new action potential in the postsynaptic neurone,can be made to do so by a process of summation. This entails a build-up of neurotransmitter in the synapse by:
1. a number of different presynaptic neurones together release enough neurotransmitter to trigger a new action potential 2. a single presynaptic neurone releases neurotransmitter many times over a short period. note: if neurotransmitter exceeds threshold value of postsynaptic neurone a new action potential is triggered.
Other chemicals
[edit | edit source]Nicotine: Similar in shape to ACh molecules and will fit into the receptors on the postsynaptic membranes, initiating action potentials were there are none, and is not broken down by enzymes and so stays for a longer time.
Organophosphorous insecticides inhibit the enzyme that breaks down ACh, allowing continuous production of action potentials, and several nerve gases work in this way.
Botulinum: A toxin produced by bacterium that prevents the release of ACh, and is usually fatal to consume.
Plant growth regulators
[edit | edit source]Plants also need communication systems providing co-ordination in their bodies and very little of it is electrical signals like those of an action potential - it is usually chemicals known as plant hormones and plant growth regulators. These chemicals can be produced in a variety of tissues in small quantities. You are only required to know about auxins, gibberellins and absicisic acid.
Auxins
[edit | edit source]Auxins are involved in determining whether a plant grows upwards or whether it branches sideways, and is synthesised in the growing tips of roots and shoots, where cells are dividing.The presence of an apical bud - an active growing point at its apex - prevents lateral, branching buds growing and is known as apical dominance. High quantities (relatively) of auxin are transported to lateral buds such that it inhibits their growth, and removal of the apical bud allows for their growth. It is thought that auxin is not the only player here - cytokinins and abscisic acid are thought to be involved.
Gibberellins
[edit | edit source]
Gibberellins are plant growth regulators and are synthesised in most places, particularly in young leaves and seeds.
Seed germination
[edit | edit source]In some seeds, gibberellins control germination to a certain extent. A seed shed from its parent lies in a state of dormancy, metabolically inactive and thus can survive in adverse conditions. The seed contains an embryo, which grows to form the new plant when the seed germinates, and is surrounded by endosperm tissue which is a food store containing starch. The outer edge is a protein-rich aleurone layer, and the whole seed is covered by a tough waterproof layer.
When the seed absorbs water, gibberellin production begins, which stimulates the synthesis of amylase by the aleurone layer. Amylase hydrolyses the starch, converting it to maltose, which is then converted to glucose and the embryo uses respires this to begin to grow. Gibberellin acts a regulator for the genes that synthesise amylase.
In stems
[edit | edit source]Gibberellins partly control the height of some plants, and is in turn controlled by their genes. The dominant allele of the tallness gene synthesises an enzyme that catalyses the synthesis of gibberellin, stimulating cell division and stem elongation.
Abscisic acid
[edit | edit source]Abscisic acid, also known as ABA, is found in almost every plant, and is synthesised in almost every cell that possesss chloroplasts or amyloplasts.
Stomatal closure
[edit | edit source]One role of ABA is responding to any stressful conditions that the plant may experience - high temperatures, low water supplies, and the plant reacts by secreting ABA, causing the stomata to close, reducing loss of water vapour from the leaf. It achieves this by increases the turgor of the guard cells by actively transporting hydrogen ions out of the guard cell, making potassium ions move into the cell. The extra potassium ions lower the solute and water potential, and water moves in via osmosis opening the stomata. It is thought that ABA binds to the proton pump and does not regulate the expression of genes like gibberellin.
Leaf abscission
[edit | edit source]Keep in mind, leaf abscission has nothing to do with absicic acid. Leaves fall because the leaf stalk breaks off from the stem. These are the stages;
- Useful substances are withdrawn from the leaves and taken into the stem, involving the breakdown of some pigments, causing the colour change of leaves.
- An abscission zone forms where the leaf stalk meets the stem - a separation layer on the leaves side, made of small cells with thin cell walls. Nearest the stem is the protective layer, made of cells whose walls contain suberin, a waxy waterproof cell.
- Enzymes then break down the cell walls at the separation layer and the leaf stalk breaks at this point
Auxin concentration is usually low in an abscised leaf, indicating it may be to blame, but high concentrations of auxin applied later can promote leaf abscission.