Radiation Oncology/Toxicity/Brain
Appearance
|
Normal tissue reactions
- Acute
- begin few hours after 1st treatment, progressively less severe with additional fractions
- mild headache, nausea
- Cause: radiation-induced permeability in blood-brain barrier
- Rx: corticosteroids
- Early-delayed
- begin 1-12 weeks after completion of RT, peak by 8 weeks, resolve spontaneously within 4 months
- transient, self-limited neurologic deterioration, somnolence, or focal encephalopathy
- headache, lethargy, exacerbation of neurologic symptoms, decline in long-term memory
- Cause: transient demyelination from damage to proliferating oligodendrocytes, plus changes in blood-brain barrier
- Rx: corticosteroids
- Late-delayed
- vary from asymptomatic white matter changes to cerebral atrophy, hemorrhagic vascular telangiectasia, neurobehavioral impairment, pituitary-hypothalamic dysfunction, radiation necrosis
- lassitude, personality changes, dementia, urinary incontinence, gait abnormalities
- Radiation necrosis: from 3 months, but usually 1-2 years after treatment. Very difficult to differentiate from tumor recurrence
- Rx: corticosteroids, surgical resection of necrotic area
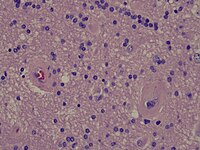
Radiation necrosis
[edit | edit source]- Brain Radiation Necrosis
-
Low power microscopy
-
Intermediate power microscopy
-
High power microscopy
Studies
[edit | edit source]External beam radiotherapy:
- Amsterdam; 2007 PMID 17555870 -- "Cerebral necrosis after 25Gy radiotherapy in childhood followed 28 years later by 54Gy radiotherapy." (Koot RW, Clin Neurol Neurosurg. 2007 Sep;109(7):607-12.)
- Case report. 34-year old with PCI 25 Gy in childhood. Then atypical meningioma treated with fractionated 54 Gy
- Outcome: 2 years later radiation necrosis, surgery confirmed
- Intergroup NCCTG/RTOG/ECOG (1986-1994)
- Randomized. 203 patients. Age >18. Included low grade astrocytoma, oligodendroglioma, or mixed oligoastrocytoma; pilocytic astrocytomas were excluded. Randomized to 50.4 Gy vs 64.8 Gy in 1.8 Gy/fx. RT technique: 2 cm margin around preoperative tumor volume, 1 cm margin for boost after 50.4 Gy.
- 5-years; 2002 PMID 11980997 — "Prospective randomized trial of low- versus high-dose radiation therapy in adults with supratentorial low-grade glioma: initial report of a North Central Cancer Treatment Group/Radiation Therapy Oncology Group/Eastern Cooperative Oncology Group study." (Shaw E et al. J Clin Oncol. 2002 May 1;20(9):2267-76.) Median F/U 6.4 years
- Toxicity: crude incidence of severe, life-threatening, or fatal radiation necrosis was 1% in low-dose vs. 6% in high-dose group (2-yr actuarial rates 2.5% vs. 5%). Radiation necrosis of brain stem leading to death recorded even at 50.4 Gy
- Washington University (1974-1976)
- 1985PMID 4070632 The risk of cerebral radionecrosis in relation to dose, time and fractionation. A follow-up study. (Marks JE, Prog Exp Tumor Res. 1985;29:210-8.)
- Brain necrosis: 18% incidence with doses > 64.8 Gy, compared to 0% with doses <57 Gy
- 1981 PMID 6260715 -- "Cerebral radionecrosis: incidence and risk in relation to dose, time, fractionation and volume." (Marks JE, Int J Radiat Oncol Biol Phys. 1981 Feb;7(2):243-52.)
- 152 patients with brain/pituitary tumors. Pathology done in 17% patients. Necrosis pathologically confirmed in 7 patients (5%), didn't vary with type of tumor. Median time to development 14 months (6 months - 2 years)
- Conclusion: no radiation necrosis <54 Gy in 30 fractions
- 1985PMID 4070632 The risk of cerebral radionecrosis in relation to dose, time and fractionation. A follow-up study. (Marks JE, Prog Exp Tumor Res. 1985;29:210-8.)
- UCSF; 1980 PMID 7007303 -- "Therapeutic irradiation and brain injury." (Sheline GE, Int J Radiat Oncol Biol Phys. 1980 Sep;6(9):1215-28.)
- Review. >100 reported cases of injury in literature analyzed, 80 evaluated. Analyzed for acute reactions, early delayed reactions, leukoencephaly, and late delayed reactions
- 20 patients with dose <50 Gy, but 17 had daily fractions 2.5 - 37.5 Gy). If dose 52 Gy in 2 Gy/fx, rate <0.5%, necrosis becomes a risk at 50-60 Gy in 2 Gy/fx
Radiosurgery:
- Cleveland / Case Western PMID 16226848 -- "12 Gy gamma knife radiosurgical volume is a predictor for radiation necrosis in non-AVM intracranial tumors." (Korytko T, Int J Radiat Oncol Biol Phys. 2006 Feb 1;64(2):419-24.)
- Retrospective, 129 pts with 198 non-AVM tumors followed with MRI every 3-6 months.
- Symptomatic radiation necrosis correlated with 12 Gy volume. Risk of asymptomatic radiation necrosis did not relate to 12 Gy volume.
Treatment
[edit | edit source]- MD Anderson; 2007 PMID 17236958 -- "Effect of bevacizumab on radiation necrosis of the brain." (Gonzalez J, Int J Radiat Oncol Biol Phys. 2007 Feb 1;67(2):323-6.)
- Retrospective. 15 patients with malignant brain tumors treated with bevacizumab (5mg/kg/2-week or 7.5mg/kg/3-week). Radiation necrosis in 8 patients. MRI studies reviewed
- Post-treatment MRI: abnormality reduction in all 8 patients. Average reduction in daily dexamethasone 8.6 mg
- Conclusion: Bevacizumab can reduce radiation necrosis, by decreasing capillary leakage and associated brain edema
Review
[edit | edit source]- Fox Chase; 1995 PMID 7677836 -- "Radiation response of the central nervous system." (Schultheiss TE, Int J Radiat Oncol Biol Phys. 1995 Mar 30;31(5):1093-112.)
- Review of anatomical, pathophysiological, and clinical aspects of radiation injury to CNS
- Spine cord: 5% radiation myelopathy probably induced at 57 - 61 Gy without chemo
- Brain: necrosis rarely <60 Gy; neurocognitive lower
Somnolence Syndrome
[edit | edit source]- Considered under category of early delayed encephalopathy
- Syndrome: somnolence (mild drowsiness to overwhelming exhaustion), low-grade fever, nausea/vomiting, and headache
- Symptoms reported in 1929 in children treated with low-energy X-rays for ringworm of scalp
- Syndrome described in 1973 in children treated with cranial RT for ALL
- Classically occurs after whole brain irradiation (after cranial RT for ALL (15-58%), and also after TBI)
- Doses as low as 12 Gy TBI have been reported to trigger it (PMID 10989470)
- Fractional dose (1.8 Gy/fx vs 1.0 Gy/fx) doesn't appear to impact incidence of clinical somnolence
- Also described after focal RT to pineal region for meningioma
- Etiology unclear, but hypothesized to be transient demyelination, possibly in the reticular activating system (RAS)
- Effects on long-term cognitive function are contradictory
- Prophylactic steroids can reduce incidence, and can be helpful in recovery. However, most children can improve spontaneously and completely without treatment
- Ankara (Turkey)(1994-1996) -- oral dexamethasone 2mg/m2 vs. 4 mg/m2
- Randomized. 32 patients with high-risk ALL. Prophylactic cranial RT 18/10. Arm 1) oral dexamethasone 2 mg/m2 during RT vs Arm 2) oral dexamethasone 4 mg/m2. Tapered in 5 days after RT
- 1998 PMID 9756169 -- "Reduced incidence of the somnolence syndrome after prophylactic cranial irradiation in children with acute lymphoblastic leukemia." (Uzal D, Radiother Oncol. 1998 Jul;48(1):29-32.)
- Outcome: Somnolence syndrome low dose 64% vs. high dose 18% (SS). Most common symptom drowsiness. Median time-to-development 4 weeks, duration of symptoms median 7 days (2-14 days). In all cases, symptoms subsided completely and spontaneously
- Conclusion: Steroids at 4 mg/m2 during cranial RT can reduce incidence of somnolence syndrome
- ? Institution -- RT dose 1 Gy/fx vs. 1.8 Gy/fx
- Randomized. 97 children with ALL, receiving cranial RT. Same chemotherapy including IT-MTX. Arm 1) 18/18 (@1 Gy/fx) vs. Arm 2) 18/10 (@1.8 Gy/fx)
- 1984 PMID 6593316 -- "The somnolence syndrome in leukemic children following reduced daily dose fractions of cranial radiation." (Littman P, Int J Radiat Oncol Biol Phys. 1984 Oct;10(10):1851-3.)
- Outcome: Clinical somnolence 58% in both groups (NS)
- Conclusion: RT dose fraction does not appear to impact incidence of somnolence
Radiation-induced moyamoya syndrome
[edit | edit source]- Snehal S Desai et al. Radiation-induced moyamoya syndrome. Int J Radiat Oncol Biol Phys. 2006 Jul 15;65(4):1222-7. (PMID: 16626890) (DOI: 10.1016/j.ijrobp.2006.01.038)
- A PubMed search of English-language articles, with radiation, radiotherapy, and moyamoya syndrome used as search key words, yielded 33 articles from 1967 to 2002.
- Patients who received RT to the parasellar region at a young age (<5 years) are the most susceptible to moyamoya syndrome.
- The incidence for moyamoya syndrome continues to increase with time, with half of cases occurring within 4 years of RT and 95% of cases occurring within 12 years.
- Patients with NF-1 have a lower radiation-dose threshold for development of moyamoya syndrome.
- Paulo Almeida et al. Moyamoya Syndrome after Radiation Therapy: a Clinical Report. Eur J Case Rep Intern Med. 2019; 6(12): 001337. (PMID: 31893204)
Radiosurgery
[edit | edit source]- See also: treatment-specific information at Radiation Oncology/CNS/Arteriovenous malformation