Introduction to Sociology/Health and Medicine
| They don’t tell you how quiet hospitals can get in the middle of the night. They don’t tell you that the sores on the skin smell strange, like from some other world. They don’t tell you that bodies can release fluids from almost any pore in rapid succession; kind of like the way tears come flying from eyes, yellow and red stuff can come out of a wrist. They don’t tell you that the whole place smells like a mixture of urine and antiseptic. They don’t tell you – though you’re not surprised – that most of the religious people going from room to room and bed to bed won’t stop to talk to you, will flinch if you try to shake their hand on the rare occasion they do stop by, and might leave miniature Bibles outside the door while you and your companion sleep inside. They don’t tell you how hard it is to hold someone and sleep in a hospital bed. They don’t tell you that the some doctors, nurses and other medical staff will bring you food, try to make your companion laugh, show you how to use the coffee machine for free as if you work there, bring you a “good” blanket from home, and harass any religious people that give you and especially your companion a hard time. They don’t tell you that other doctors, nurses, and other medical staff will try to get you to leave, will avoid contact with your body and your eyes just in case you have caught your companion’s condition and they have already forgot how transmission works, will be overheard saying things like, “Well, he probably asked for it,” or will ask you to close the door to your companion’s room because it might upset people. They don’t tell you that when you feed someone ice chips you need to move slow and softly and be ready to hold them if they start to choke on something even that small. They don’t tell you what it feels like to watch your first love die from AIDS. Even though they don't tell you any of these things, I can promise you that you’ll never forget it no matter how hard you try. |
Introduction
[edit | edit source]
The World Health Organization (WHO) defines health as "a state of complete physical, mental and social well-being, and does not consist only of the absence of disease or infirmity" (source) Though this is a useful definition, some would consider it idealistic and non-realistic because using the WHO definition classifies 70-95% of people as unhealthy. There can also be other definitions of health, e.g. statistical (systolic blood pressure and diastolic blood pressure) and functional (ability to carry out Activities of Daily Living or ADLs). The WHO definition also overlooks the fact that several factors influence both the definition of health and standards of health.

What it means to be healthy can vary from culture to culture and is often connected with advances in technology and cultural patterns of race, class, gender, and sexual inequalities. In some cultures, larger body sizes are seen as a sign of healthiness as it indicates an individual has a preponderance of food. In other cultures, largeness is more closely associated with unhealthy lifestyles (e.g., lack of exercise, poor eating habits, etc.). Advances in technology have also expanded the idea of what it means to be healthy. What are understood today to be healthy practices were not emphasized prior to clear understandings of disease and the contributions of lifestyles to health, and some practices advanced as "healthy" today are the result of cultural beliefs that benefit some at the expense of others. Finally, sociologists have demonstrated that access, utilization, education, and practices related to health and well being are heavily influenced by (and often seemingly determined by) prevailing cultural norms, beliefs, and patterns that often have little or nothing to do with physiological health.
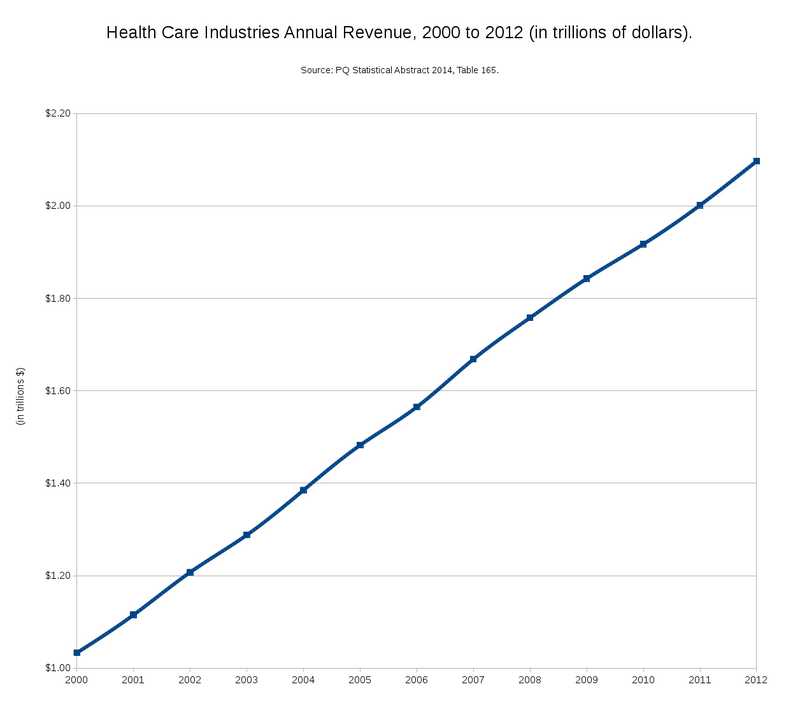
Health care (or healthcare) is an industry associated with the prevention, treatment, and management of illness along with the promotion of mental and physical well-being through the services offered by the medical and allied health professions. Healthcare is one of the world's largest and fastest-growing industries, consuming over 10 percent of gross domestic product of most developed nations. In 2000, health care costs paid to hospitals, doctors, diagnostic laboratories, pharmacies, medical device manufacturers and other components of the health care system, consumed an estimated 14 percent of the gross national product of the United States, the largest of any country in the world. For the G8 countries (eight of the most developed countries in the world) the average is about nine percent. Importantly, this may be due to the United States' interesting position as the only G8 and highly developed country that, since The Health Maintenance Organization Act of 1973, utilizes a private, for profit system of managed care rather than a public good, non-profit system of health promotion. In fact, the U.S. healthcare system generally costs more, produces equal or worse outcomes, incentivizes treatment over prevention, emphasizes cures over health, values quantity over quality of life, uses a lot of advanced technologies, and is heavily determined by "market forces" in comparison to healthcare systems (some nonprofit and some for profit) in other developed countries.[1]
Exploring patterns like those noted above in relation to U.S. healthcare, Medical Sociology is concerned with the distribution of healthcare services globally, in particular inequalities in healthcare, and how conceptions of health have changed over time.
Health Disparities
[edit | edit source]
While technology has advanced the practice of medicine and generally improved health, not all people have the same access to health care or the same quality of health care. According to the Health Resources and Services Administration of the U.S., health disparities are the "population-specific differences in the presence of disease, health outcomes, or access to health care" (source). Of particular interest to sociologists are the differences in health and quality of health care across racial, socioeconomic, ethnic, gender, and sexual groups.
In the United States, health disparities are well documented in racial minority populations such as African Americans, Native Americans, Asian Americans, and Hispanics. When compared to European Americans, these minority groups have higher incidents of chronic diseases, higher mortality, and poorer health outcomes. Among the disease-specific examples of racial and ethnic disparities in the United States is the cancer incidence rate among African Americans, which is 10 percent higher than among European Americans and generally linked to the environmental conditions of predominantly racial minority neighborhoods. In addition, American adults of African and Hispanic lineage have approximately twice the risk of developing diabetes than American adults of European lineage, which often reflects the lack of access to quality foods and healthcare resources within predominantly racial minority neighborhoods. Minorities also have higher rates of cardiovascular disease, HIV/AIDS, and infant mortality than whites, which suggests the lack of preventative services and education in predominantly racial minority neighborhoods and schools may play an important role. There are also substantial differences in health based on social class or socioeconomic status, which have also been linked to neighborhood concentration and environmental effects.[2] As of 2009, diseases that were common only in the developed world (e.g., toxocariasis, cysticercosis, chagas, and cytomegalovirus) were becoming a serious concern among economically disadvantaged populations in the U.S.[2] Building on these insights, sociologists and public health researchers have documented a wide variety of racial and economic health disparities tied to neighborhood and environmental contexts,[3][4][5][6] and have even begun requiring graduate courses and training workshops on neighborhood contexts for public health, epidemiological, and medical sociology researchers.
Researchers have also documented significant health disparities within gender and sexual minority populations in the United States.[7] In terms of gender, for example, researchers have found that women and trans people experience significantly different treatment from health care providers, and often experience more chronic conditions throughout the life course. Further, these researchers have noted the tendency for medical research to prioritize illnesses that are more common in heterosexual men while downplaying, ignoring, and stigmatizing conditions that are more common among other gender and sexual groups. In terms of sexualities, for example, researchers have documented the systematic exclusion of non-heterosexual healthcare needs, priorities, and concerns throughout medical history, training programs, and certification processes,[8] and sexual minorities regularly report primarily negative interactions with healthcare providers in the United States.[9] Further, medical history is littered with example of labeling women's natural experiences and bodily functions (especially during times of women's rights movement activity and success) in medical terms that serve to stigmatize, control, and devalue women's health and well-being.[10] FInally, historical records reveal the use of medical authority and technologies to demonize, stigmatize, and justify the institutionalization and arrest of sexual minorities throughout the last century.[11] In all such cases, gender and sexual minorities regularly experience disparate outcomes, experiences, and relationships as a result of healthcare systems that treat them differently.



Causes of Health Disparities
[edit | edit source]There is debate about what causes health disparities between dominant and subordinate groups. However, it is generally accepted that disparities can result from three main areas:
- From the differences in socioeconomic and environmental characteristics of different ethnic and racial groups. For instance, American Africans and Hispanics tend to live in poorer neighborhoods that are near to industrial areas and are older than new suburban subdivisions. Industrial pollutants and lead-paint, common in older homes, can both lead to increased incidents of disease. Similarly, gender and sexual minorities are more likely to be displaced from their homes at earlier ages (e.g., with less symbolic and economic capital) than other members of society.[12]
- From the barriers certain minority groups encounter when trying to enter into the health care delivery system.
- From the quality of health care different minority groups receive.
Most attention on the issue has been given to the health outcomes that result from differences in access to medical care among groups and the quality of care different groups receive. Reasons for disparities in access to health care are many, but can include the following:
- Lack of insurance coverage. Without health insurance, patients are more likely to postpone medical care, more likely to go without needed medical care, and more likely to go without prescription medicines. Minority groups in the United States lack insurance coverage at higher rates than members of dominant groups.
- Lack of a regular source of care. Without access to a regular source of care, patients have greater difficulty obtaining care, fewer doctor visits, and more difficulty obtaining prescription drugs. Compared to whites, minority groups in the United States are less likely to have a doctor they go to on a regular basis and are more likely to use emergency rooms and free or reduced rate, government subsidized clinics as their regular source of care.
- Lack of financial resources. Although the lack of financial resources is a barrier to health care access for many Americans, the impact on access appears to be greater for minority populations.
- Structural barriers. Structural barriers to health care include poor transportation, an inability to schedule appointments quickly or during convenient hours, and excessive time spent in the waiting room, all of which affect a person's ability and willingness to obtain needed care.
- The health financing system. The Institute of Medicine in the United States says fragmentation of the U.S. health care delivery and financing system is a barrier to accessing care. Racial and ethnic minorities are more likely to be enrolled in health insurance plans which place limits on covered services and offer a limited number of health care providers.
- Scarcity of providers. In inner cities, rural areas, and communities with high concentrations of minority populations, access to medical care can be limited due to the scarcity of primary care practitioners, specialists, and diagnostic facilities. In addition more private practices are putting limits on the number of medicaid and medicare patients that they will accept because these programs reimburse at a much lower percentage than private insurers. Finding physicians who accept Medicaid and Medicare is becoming increasingly difficult.
- Linguistic barriers. Language differences restrict access to medical care for minorities in the United States who are not English-proficient.
- Low Health literacy. This is where patients have problems obtaining, processing, and understanding basic health information. For example, patients with a poor understanding of good health may not know when it is necessary to seek care for certain symptoms. Similarly, they may not understand the medical jargon that is used by health professionals and, consequently, are unable to accurately follow medical instructions. While problems with health literacy are not limited to minority groups, the problem can be more pronounced in these groups than in whites due to socioeconomic and educational factors.
- Lack of diversity in the health care workforce. Cultural differences between predominantly white health care providers and minority patients is also often cited as a barrier to health care. Only 4% of physicians in the United States are African American; Hispanics represent just 5%. These percentages are much lower than these groups' respective proportions of the United States population.
- Provider discrimination. This is where health care providers either unconsciously or consciously treat certain racial and ethnic patients differently than they treat their white patients. Some research suggests that minorities are less likely than whites to receive a kidney transplant once on dialysis or to receive pain medication for bone fractures. Critics question this research and say further studies are needed to determine how doctors and patients make their treatment decisions. Others argue that certain diseases cluster by ethnicity and that clinical decision making does not always reflect these differences.


Examples of Health Disparities
[edit | edit source]There are a number of ways in which health disparities play out based on different systems of stratification. Health disparities resulting from economic stratification are wide-ranging. Poorer women have reduced access to mammograms to detect breast cancer, even when they are better candidates for screening.[13] Wealthier people live longer than poorer people. Wealthier people in the U.S. today live about 4.5 years longer than poorer people (79.2 vs. 74.7, respectively).[14] Additionally, affluent and more educated people are more likely to take advantages of advances in medical science and technology and have seen a more rapid decline in smoking rates, which directly improves health.[14] Disparities in health care between the rich and poor are not inevitable - they are directly correlated with disparities in wealth. The differential and unequal treatment of the rich and poor follows the gap between the rich and the poor: From 1966 to 1980, socioeconomic disparities declined in tandem with a decline in mortality rates, but the disparity has since increased as income stratification has, and as our healthcare model has become mostly private, for profit, and insurance based.[14]
Financial access to health care is not the only factor that affects health; poorer people are generally less likely to exercise, resulting in overall poorer health as well.[15] This is probably due to fewer opportunities to exercise and less access to safe, clean exercise facilities. Poorer individuals also live in more dangerous neighborhoods and are more likely to eat unhealthy food (or lack the resources necessary to prepare healthy food they acquire) and engage in risky or unhealthy behavior (often as a result of a lack of options for healthy and less risky behaviors within their environments), all of which contributes to poorer health.[14][16]
As noted above, researchers also find health disparities based on gender and sexual stratification. One study found that women are less likely than men to be recommended for knee replacement surgery, even when they have the same symptoms.[17] While it was unclear what role the sex of the recommending physicians played, the authors of this study encourage women to challenge their doctors in order to get care equivalent to men. Expanding on examples like this, researchers have noted that the ways medical professionals approach sexual and gender minorities are often heavily sexualized and gendered, which creates barriers for gender and sexual minorities - even those with the economic and educational resources to acquire care.[18][9]
Health disparities based on race also exist. Similar to the difference in life expectancy found between the rich and the poor, affluent white women live 14 years longer in the U.S. (81.1 years) than poor black men (66.9 years).[14][19] There is also evidence that blacks receive less aggressive medical care than whites, similar to what happens with women compared to men.[14] Black men describe their visits to doctors as stressful and report that physicians do not provide them with adequate information to implement the recommendations they are given, similar to gender and sexual minorities.[19] Another contributor to the overall worse health of blacks is the incident of HIV/AIDS - the rate of new AIDS cases is 10 times higher among blacks than whites and blacks are 20 times as likely to have HIV/AIDS as are whites, which is generally due to the structural violence (e.g., poverty, lack of health education, lack of access to medical care, and lack of sexual education) plaguing contemporary African-American communities.[20][21]
Paying for Medical Care
[edit | edit source]As noted in the previous section, disparities in health care are often related to an individual's or a group's ability to pay for health care. This section discusses the costs of healthcare and the different approaches to health care that have been taken by governments around the world.
Health Insurance
[edit | edit source]Health insurance is a type of insurance whereby the insurer pays the medical costs of the insured if the insured becomes sick due to covered causes or accidents. The insurer may be a private organization or a government agency. According to the 2005 United States Census Bureau, approximately 85% of Americans have health insurance. Approximately 60% obtain health insurance through their place of employment or as individuals and various government agencies provide health insurance to 25% of Americans. Despite the claims of the Patient Protection and Affordable Care Act, however, it is important to remember that researchers have demonstrated that access to health insurance will have a limited impact on health disparities due to the importance of varied types of social, psychological, material, symbolic, and political resources in the overall construction, maintenance, and challenge of health inequalities.[22]
While the rising cost of health care is debated, some contributing causes are accepted. Aging populations require more health care as a result of increased life expectancy. Advances in medical technology have arguably driven up the prices of procedures, especially cutting edge and experimental procedures. Poor health choices also increase health care costs by increasing the incident of disease and disability. Preventable health issues are related to:
- insufficient exercise
- unhealthy food choices
- excessive alcohol consumption
- smoking
- obesity (more on this below)
In theory, people could lower health insurance prices by exercising, eating healthy food, and avoiding addictive substances that are damaging to the body. Healthier lifestyles protect the body from disease, and with fewer diseases, there would be fewer health care related expenses, but healthier lifestyles rely upon the opportunity to possess favorable economic resources and neighborhood location (e.g., exercise, food choices, obesity), and the ability to avoid (or find alternate ways to manage) experiencing continuous stress exposure, traumatic events, and structural violence (e.g., alcohol and cigarette consumption).
Another element of high health care costs is related to the private management of healthcare by large corporations. While this is discussed in greater detail below, it is worth noting that corporate profits have also played a role in increased health care premiums.

Private Insurance and Free-Market Health Care
[edit | edit source]Two types of health insurance have developed in modern society: private health insurance (or free-market) models and publicly funded health insurance models. The benefits and drawbacks of each of these models are discussed in this and the following section.
Private insurance refers to health insurance provided by a non-governmental organization, usually a privately owned or publically traded corporation. Private insurance as the primary provider of health care in a developed nation is really only found in the United States as of 1973. It is important to note that while the United States is the most private of any system, there is a substantial public component. Of every dollar spent on health care in the United States, 44 cents comes from some level of government. In addition, government also increases private sector costs by imposing licensing and regulatory barriers to entry into both the practice of medicine and the drug trade within America. Private practitioners also face inflated costs through the government's use of protectionist measures against foreign companies, to uphold the intellectual property rights of the U.S. pharmaceutical industry.
Advocates of the private model argue that this approach to health care has the following benefits:
- Some economists argue that the free market is better able to allocate discretionary spending where consumers value it the most. There is variation among individuals about how much they value peace of mind and a lower risk of death. For example, while a public-funded system (see below) might decide to pay for a pap smear only once every five years if the patient was not positive for the human papilloma virus based on cost efficiency, in a private system a consumer can choose to be screened more often and enjoy the luxury of greater peace of mind and marginally reduced risk. When evaluating the pool of current medical spending available to fund cost effective care for the uninsured, this discretionary spending might be moved to non-medical luxury goods. Also, since current private plans are not very good at limiting spending to cost effective procedures and schedules, those consumers exploiting this will view the transition to a public system as a reduction in their compensation or benefits, and will question whether a society that will allow them to buy a better car or a European vacation, but not better health care, is truly free.
- Advocates also point to the remarkable advances in medical technology that have accompanied the private insurance/free-market approach to health care. When health care is privately funded, the opportunity for making large amounts of money is an attractive proposition for researchers in medical technology and pharmaceuticals. Thus, the private insurance system, while it may not provide adequate care for everyone (see the criticisms below), does provide cutting edge technology for those who can afford it.
- Advocates also argue that private industry is more efficient than government, which can be quite susceptible to bloat and bureaucracy. However, as is discussed below, this is not always true.
Despite these possible benefits, the private insurance approach is not without its drawbacks. Following are some of the more common criticisms of the private health insurance approach to health care:
- As noted above, private insurance can be a boon to those who can afford the cutting edge technology. But the flipside to this boon is that the United States, the only mostly-private health delivery system in a developed country, is below average among developed nations by almost every health measure, including: infant mortality, life expectancy, chronic diseases and cancer survival rates.[23] As evidence of this, people in lower socioeconomic classes in the US are significantly more likely to contract a preventable disease than are people in higher socioeconomic classes, which is not the case in Canada, where they have universal healthcare.[24] This is directly attributable to reduced access to healthcare in the US for those with less money.
- More than half of the people with chronic conditions in the US regularly skip pills and doctors' appointments for conditions like diabetes, heart disease, cancer, and depression because of the cost of the care.[25]
- Another significant criticism of the private system is that it ends up being more costly than publicly funded systems. In 2001 the United States government spent $4,887 per person on health care. That is more than double the rate of any other G8 country, except Japan which spends close to $2,627 per capita annually. Considering private insurers are supposed to cover the majority of health care costs in the U.S., it is somewhat surprising that the United States spends a greater fraction of its national budget on health than Canada, Germany, France, or Japan. One explanation for the higher health care costs in the U.S. is the billing approach: in the U.S., many doctors work on a fee-for-service basis, which means they earn more if they do more tests or are consulted more frequently. In contrast, doctors who are salaried have no financial incentive to perform unnecessary tests. This was the explanation given for the wide disparity in Medicare spending for patients in the last two years of their lives at top teaching hospitals: per patient costs at UCLA were $93,000, but only $53,000 at the Mayo Clinic. When doctors are salaried, they are not inclined to perform unnecessary tests just to increase their income, which is what doctors using fee-for-service approaches do.[26] The quality of care and patient life expectancy did not differ between these two hospitals, despite the substantial difference in costs.
- Most experts believe that significant market failure occurs in health markets, thereby leading free market insurance models to operate inefficiently. The consumers of health care are vastly less knowledgeable than the medical professionals they buy it from. An individual is especially less likely to make rational choices about his/her own health care in a case of emergency. The extreme importance of health matters to the consumer adds to the problem of the information gap. This gives the medical profession the ability to set rates that are well above free market value. The need to ensure competence and qualifications among medical professionals also means that they are inevitably closely controlled by professional associations that can exert monopolistic control over prices. Monopolies are made even more likely by the sheer variety of specialists and the importance of geographic proximity. Patients in most markets have no more than one or two heart specialists or brain surgeons to choose from, making competition for patients between such experts very limited.
- In theory when a government sets billing rates it can negotiate with the professional societies with equal heft and knowledge, reaching a total cost that is closer to the ideal than an unregulated market. In private insurance systems, each insurance company is responsible for negotiating its own salaries. A possible result of this approach is the higher pay in doctors' salaries. Doctors' salaries do tend to be much lower in public systems. For instance, doctors' salaries in the United States are twice those in Canada.
- The private insurance or free-market approach also fails to provide an efficient delivery for health care because prevention is such an essential component, but one that most people misjudge. Screening for diseases such as cancer saves both lives and money, but there is a tendency within the general population to not correctly assess their risk of disease and thus to not have regular check ups. Many people are only willing to pay a doctor when they are sick, even though this care may be far more expensive than regular preventative care would have been. Delaying treatment until the condition is too severe to be treated can result, often with serious and lamentable consequences.[27] The one exception is when extensive publicity, such as that for mammograms, is undertaken. Making regular appointments cheaper, or even free (as is done in public systems), has been shown to reduce both rates of illness and costs of health care. Conversely, placing the cost of a visit to a general practitioner too low will lead to excessive visits wasting both a patient's and a doctor's time. Thus while some experts believe free doctor visits produce ideal results, most believe that forcing people to pay some fraction of the cost of an appointment is better.
- When a claim is made, particularly for a sizeable amount, the use of paperwork and bureaucracy can allow insurance companies to avoid payment of the claim or, at a minimum, greatly delay it. Some people simply give up pursuing their claims with their insurance provider. This is a cost-cutting technique employed by some companies; fighting claims legally is actually less expensive in some instances than paying the claims outright.
- Insurance companies usually do not announce their health insurance premiums more than one year in advance. This means that, if one becomes ill, he or she may find that the premiums have greatly increased. This largely defeats the purpose of having insurance in the eyes of many. However, this is not a concern in many group health plans because there are often laws that prevent companies from charging a single individual in the plan more than others who are enrolled in the same insurance plan.
- Health insurance is often only widely available at a reasonable cost through an employer-sponsored group plan. This means that unemployed individuals and self-employed individuals are at an extreme disadvantage and will have to pay for more for their health care.
- Experimental treatments or particularly expensive drugs are often not covered.[28] This practice is especially criticized by those who have already tried, and not benefited from, all standard medical treatments. Because insurance companies can avoid paying claims for experimental procedures, this has lead some insurers to claim that procedures are still experimental well after they have become standard medical practice. This phenomenon was especially prevalent among private insurance companies after organ transplants, particularly kidney transplants, first became standard medical practice, due to the tremendous costs associated with this procedure and other organ transplantation. This approach to avoiding paying premiums can also undermine medical advances.
- Health Maintenance Organizations or (HMO) types of health insurance are often criticized for excessive cost-cutting policies that include accountants or other administrators making medical decisions for customers. Rather than allowing such decisions to be made by health care professionals who know which procedures or treatments are necessary, these health plan administrators are dictating medical practice through their refusal to cover claims.
- As the health care recipient is not directly involved in payment of health care services and products, they are less likely to scrutinize or negotiate the costs of the health care they receive. To care providers (health care professionals, not the insurers), insured care recipients are viewed as customers with relatively limitless financial resources who do not consider the prices of services. To address this concern, many insurers have implemented a program of bill review in which insured individuals are allowed to challenge items on a bill (particularly an inpatient hospital bill) as being for goods or services not received. If a challenge is proven accurate, insured individuals are awarded with a percentage of the amount that the insurer would have otherwise paid for this disputed item or service.
Concerns about health insurance are prevalent in the United States. A June 2005 survey of a random national sample by the Kaiser Family Foundation found that twice as many Americans are more worried about rising health care costs than losing their job or being the victim of a terrorist attack (source). Healthcare changes in the United States, however, are typically rife with conflict, slow to progress, and dominated by concerns about profits rather than patients, which often leads to a highly fractured and conflict-oriented approach with little room for significant changes except over vast periods of time (see debates surrounding Social Security, the Hill-Burton Act, the EMTALA, and the Patient Protection and Affordable Care Act for examples.
Publicly Funded Health Care
[edit | edit source]An alternative to private health insurance and the free-market approach to health care is publicly funded health care. Publicly funded medicine is health care that is paid wholly or mostly by public funds (i.e., taxes). Publicly funded medicine is often referred to as socialized medicine by its opponents, whereas supporters of this approach tend to use the terms universal healthcare, single payer healthcare, or National Health Services. It is seen as a key part of a welfare state.

This approach to health care is the most common and popular among developed (and developing) nations around the world today. The majority of developed nations have publicly funded health systems that cover the great majority of the population. For some examples, see the British National Health Service, medicare Canada and medicare Australia.
Even among countries that have publicly funded medicine, different countries have different approaches to the funding and provision of medical services. Some areas of difference are whether the system will be funded from general government revenues (e.g. Italy, Canada) or through a government social security system (France, Japan, Germany) on a separate budget and funded with special separate taxes. Another difference is how much of the cost of care will be paid for by government or social security system, in Canada all hospital care is paid for by the government while in Japan patients must pay 10 to 30% of the cost of a hospital stay. What will be covered by the public system is also important; for instance, the Belgian government pays the bulk of the fees for dental and eye care, while the Australian government covers neither.
The United States has been virtually alone among developed nations in not maintaining a publicly-funded health-care system since South Africa adopted a publicly-funded system after toppling its apartheid regime. However, a few states in the U.S. have taken serious steps toward achieving this goal, most notably Minnesota. Other states, while not attempting to insure all of their residents strictly speaking, cover large numbers of people by reimbursing hospitals and other health-care providers using what is generally characterized as a charity care scheme, which often includes levies. A 2007 New York Times/CBS Poll found that a majority of Americans support some form of universal healthcare (59%), and just as many Americans support it even if it means raising their taxes.[29] Support is mixed between Democrats, Republicans, and Independents: 63% of Democrats support universal healthcare, 49% of Independents do, and 30% of Republicans do.
Publicly funded medicine may be administered and provided by the government, but in some systems that is not an obligation: there exist systems where medicine is publicly funded, yet most health providers are private entities. The organization providing public health insurance is not necessarily a public administration, and its budget may be isolated from the main state budget. Likewise, some systems do not necessarily provide universal healthcare, nor restrict coverage to public health facilities.
Proponents of publicly funded medicine cite several advantages over private insurance or free-market approaches to health care:
- Publicly funded approaches provide universal access to health care to all citizens, resulting in equality in matters of life and death.
- Publicly funded health care reduces contractual paperwork.
- Publicly funded health care facilitates the creation of uniform standards of care.
- Publicly funded health care may help reduce illnesses associated with job loss. As many people in the US rely on their jobs for health insurance, losing their jobs increases stress and, as a result, increases illness.[30]
- It is also the case that publicly funded systems result in a reduction in the percentage of societal resources devoted to medical care; meaning public systems cost less than private systems.
Publicly funded health care is not without its criticisms. Some purported disadvantages of the public system include:
- Some critics argue there is a greater likelihood of lower quality health care than privately funded systems. However, because of the universal accessibility of health care, this claim is generally not true.[23]
- Another criticism of publicly funded health care is that there is less motivation for medical innovation and invention and less motivation for society's most skilled people to become doctors, because of the lower amount of monetary compensation.
- Price no longer influences the allocation of resources, thus removing a natural self-corrective mechanism for avoiding waste and inefficiency (though the redundancy of the private system - competing insurers - often results in more inefficiency than a single, public system).
- Health care workers' pay is often not related to quality or speed of care. Thus very long waits can occur before care is received.
- Because publicly funded medicine is a form of socialism, many of the general concerns about socialism can be applied to this approach.
- People are afraid that they can't choose their own doctor. The state chooses for them. This also tends to be an over-exaggerated and ill-founded concern as there is some degree of freedom in choosing medical practitioners in public systems.
Parallel Public/Private Systems
[edit | edit source]Almost every country that has a publicly funded health care system also has a parallel private system, generally catering to the wealthy. While the goal of public systems is to provide equal service, the egalitarianism tends to be closer to partial egalitarianism. Every nation either has parallel private providers or its citizens are free to travel to a nation that does, so there is effectively a two-tier healthcare system that reduces the equality of service. Since private providers are typically better paid, those medical professionals motivated by remunerative concerns migrate to the private sector while the private hospitals also get newer and better equipment and facilities. A number of countries such as Australia attempt to solve the problem of unequal care by insisting that doctors divide their time between public and private systems.
Proponents of these parallel private systems argue that they are necessary to provide flexibility to the system and are a way to increase funding for the health care system as a whole by charging the wealthy more. Opponents believe that they are allowed to exist mainly because politicians and their friends are wealthy and would prefer better care. They also argue that all citizens should have access to high quality healthcare. The only country not to have any form of parallel private system for basic health care is Canada. However, wealthy Canadians can and travel to the United States for care.
Also, in some cases, doctors are so well paid in both systems that prestige is often more important to them than remuneration. This is very much the case in the United Kingdom where private medicine is seen as less prestigious than public medicine by much of the population. As a result, the best doctors tend to spend the majority of their time working for the public system, even though they may also do some work for private healthcare providers. The British in particular tend to use private healthcare to avoid waiting lists rather than because they believe that they will receive better care from it.
Difficulties of analysis
[edit | edit source]Cost-benefit analysis of healthcare is extremely difficult to do accurately, or to separate from emotional entanglement. For instance, prevention of smoking or obesity is presented as having the potential to save the costs of treating illnesses arising from those choices. Yet, if those illnesses are fatal or life shortening, they may reduce the eventual cost to the system of treating that person through the rest of their life, and it is possible that they will die of an illness every bit as expensive to treat as the ones they avoided by a healthy lifestyle.
This has to be balanced against the loss of taxation or insurance revenue that might come should a person have a longer productive (i.e. working and tax or insurance-paying) life. The cost-benefit analysis will be very different depending on whether you adopt a whole-life accounting, or consider each month as debits and credits on an insurance system. In a system financed by taxation, the greatest cost benefit comes from preserving the working life of those who are likely to pay the most tax in the future, i.e. the young and rich.
Few politicians would dare to present the big picture of costs in this way, because they would be condemned as callous. Nevertheless, behind the scenes, a responsible government must be performing cost analysis in order to balance its budget; it is not likely, however, to take the most purely cost effective route. It may choose to provide the best health care according to some other model, but the cost of this still must be estimated and funded, and there is no uncontroversial definition of best.
In producing a definition of quality of healthcare, there is an implication that quality can be measured. In fact, the effectiveness of healthcare is extremely difficult to measure, not only because of medical uncertainty, but because of intangible quantities like quality of life. This is likely to lead to systems that measure only what is easy to measure (such as length of life, waiting times or infection rates). As a result, the importance of treating chronic, but non-fatal conditions, or of providing the best care for the terminally ill may be reduced. Thus, it is possible for personal satisfaction with the system to go down, while metrics go up.
Behavior and Environmental Influences on Health
[edit | edit source]The following sections explore some of the ways behaviors and environment can impact human health.
Smoking
[edit | edit source]The Centers for Disease Control and Prevention describes tobacco use as "the single most important preventable risk to human health in developed countries and an important cause of premature death worldwide" (source). A person's increased risk of contracting disease is directly proportional to the length of time that a person continues to smoke as well as the amount smoked. However, if someone stops smoking the risks of developing diseases steadily decline, although gradually, as the damage to their body is repaired.
The main health risks from tobacco smoking pertain to diseases of the cardiovascular system, in particular smoking is a major risk factor for: myocardial infarction (heart attack); diseases of the respiratory tract, such as Chronic Obstructive Pulmonary Disease (COPD) and emphysema; and cancer, particularly lung cancer and cancers of the larynx and tongue. Prior to World War I, lung cancer was considered to be a rare disease, one most physicians would never see during their career. With the postwar rise in popularity of cigarette smoking came a virtual epidemic of lung cancer.
Alcohol
[edit | edit source]Alcoholism is a dependency on alcohol characterized by craving (a strong need to drink), loss of control (being unable to stop drinking despite a desire to do so), physical dependence and withdrawal symptoms, and tolerance (increasing difficulty of becoming drunk).
Although acceptance of the American Disease Model is not without controversy, the American Medical Association, the American Psychiatric Association, the American Hospital Association, the American Public Health Association, the National Association of Social Workers, the World Health Organization, and the American College of Physicians have all classified alcoholism as a disease.
In a 1992 JAMA article, the Joint Committee of the National Council on Alcoholism and Drug Dependence and the American Society of Addiction Medicine published this definition for alcoholism: "Alcoholism is a primary chronic disease with genetic, psychosocial, and environmental factors influencing its development and manifestations. The disease is often progressive and fatal. It is characterized by impaired control over drinking, preoccupation with the drug alcohol, use of alcohol despite adverse consequences, and distortions in thinking, mostly denial. Each of these symptoms may be continuous or periodic."
Symptoms of a person's dependence on alcohol may include, but are not limited to, a feeling of necessity in regards to consumption of alcohol, or an inability to resist alcohol if offered. Though these symptoms often arise from a physical dependence on the substance, it is not uncommon for individuals, especially teenagers and adolescents between the ages of fifteen and twenty, to rely on alcohol as a means of social interaction. If a person cannot refuse alcohol in the presence of others, insists on drinking alcohol excessively for fear of alienation and neglect, or feels they cannot socially interact with others unless under the influence then this person is considered socially dependent on the substance. These traits can be noticed in individuals who relocate (such as students attending a new university) whereby an individual with no past history of alcohol consumption begins to consume alcohol in order to associate and relate to others. Social dependence, though not physically threatening in early stages, can lead to physical dependence if the person cannot control their urges and more so their reasons for drinking.
The causes for alcohol abuse and dependence cannot be easily explained, but the long-standing, unscientific prejudice that alcoholism is the result of moral or ethical weakness on the part of the sufferer has been largely altered. Recent polls show that 90% of Americans currently believe that alcoholism is, in fact, a disease (source?). Of the two thirds of the North American population who consume alcohol, 10% are alcoholics and 6% consume more than half of all alcohol. Stereotypes of alcoholics are often found in fiction and popular culture. In modern times, the recovery movement has led to more realistic portraits of alcoholics and their problems.
The social problems arising from alcoholism can include loss of employment, financial problems, marital conflict and divorce, convictions for crimes such as drunk driving or public disorder, loss of accommodation, and loss of respect from others who may see the problem as self-inflicted and easily avoided. Exhaustive studies, including those by author Wayne Kritsberg, show that alcoholism affects not only the addicted but can profoundly impact the family members around them. Children of alcoholics can be affected even after they are grown. This condition is usually referred to as The Adult Children of Alcoholics Syndrome. Al-Anon, a group modelled after Alcoholics Anonymous, offers aid to friends and family members of alcoholics.
Moderate Drinking
[edit | edit source]Of course, not everyone who consumes alcohol is an alcoholic or is at danger of becoming an alcoholic. In fact, there is some debate as to whether there are some benefits derived from moderate consumption of alcohol. The controversy over moderate drinking is an ongoing debate about the claimed benefit or harm to human health from moderate consumption of alcoholic beverages. Moderate consumption typically means the consumption of 1 to 3 drinks of an alcoholic beverage a day; the number varies with age and gender. There is wide consensus that over-drinking is harmful: alcohol damages human cells and organs such as the brain, liver and kidney.
Many studies show that consumers of up to 3 drinks a day have a 10% to 40% lower risk of coronary heart disease than those who abstain. Rimm et al.[31] predict a 24.7% decrease in the risk of coronary heart disease based upon 30g alcohol/day.
Critics of moderate drinking claim that any benefits are far outweighed by the possible consequences of over consumption and that these benefits can be had by less risky means. Scientists also note that studies supporting the benefits of moderate drinking do not control for other factors, such as lifestyle differences between moderate drinkers and nondrinkers. There is evidence that moderate drinkers are more affluent than nondrinkers and as such lead lifestyles that are more conducive to good health in general.
Research on the effects of moderate drinking is in its early stages. No long term studies have been done and control groups would be difficult to establish because of the many variables. The current medical recommendation[32] regarding being a moderate drinker is that it is "not only meaningless but also irresponsible" to become a moderate drinker if you don't already drink given that the many obvious health hazards of alcohol outweigh "the benefits of alcohol [which] are small and ill-understood" particularly when so many other cardiovascular treatments are available (p. 651).
Effects of Fetal Alcohol Exposure
[edit | edit source]Fetal alcohol exposure is regarded by researchers as the leading known cause of mental and physical birth defects, surpassing both spina bifida and Down syndrome, producing more severe abnormalities than heroin, cocaine, or marijuana, and is the most common preventable cause of birth defects in the United States (source).
It can cause mental retardation, facial deformities, stunted physical and emotional development, behavioral problems, memory deficiencies, attention deficits, impulsiveness, an inability to reason from cause to effect; a failure to comprehend the concept of time; and an inability to tell reality from fantasy. Secondary disabilities develop over time because of problems fitting into the environment.
Researchers believe that the risk is highest early in the pregnancy, but there are risks throughout because the fetus' brain develops throughout the entire pregnancy. No amount of alcohol, during any trimester, is absolutely safe.
Obesity
[edit | edit source]
Obesity is a condition in which the natural energy reserve of humans, which is stored in fat tissue, is expanded far beyond usual levels to the point where it impairs health. While cultural and scientific definitions of obesity are subject to change, it is accepted that excessive body weight predisposes to various forms of disease, particularly cardiovascular disease.
There is continuous debate over obesity, at several levels. The scientific evidence informing these debates is more contradictory than most simple arguments assume. Statistics demonstrating correlations are typically misinterpreted in public discussion as demonstrating causation, a fallacy known as the spurious relationship.
In several human cultures, obesity is (or has been) associated with attractiveness, strength, and fertility. Some of the earliest known cultural artifacts, known as Venuses, are pocket-sized statuettes representing an obese female figure. Although their cultural significance is unrecorded, their widespread use throughout pre-historic Mediterranean and European cultures suggests a central role for the obese female form in magical rituals and implies cultural approval of (and perhaps reverence for) this body form.
Obesity functions as a symbol of wealth and success in cultures prone to food scarcity. Well into the early modern period in European cultures, it still served this role. Contemporary cultures which approve of obesity, to a greater degree than European and Western cultures, include African, Arabic, Indian, and Pacific Island cultures. The implication of these cultural variations in attitudes toward obesity is that ideal body shape is culturally relative. Another illustration of this is the finding that feminists are less likely to consider "ultra-thin" the ideal body image than non-feminists, indicating the culture and philosophy of feminism countermands the effects of popular media.[33] In Western cultures, obesity has come to be seen more as a medical condition than as a social statement.
Various stereotypes of obese people have found their way into expressions of popular culture. A common stereotype is the obese character who has a warm and dependable personality, presumedly in compensation for social exclusion, but equally common is the obese vicious bully. Gluttony and obesity are commonly depicted together in works of fiction. It can be argued that depiction in popular culture adds to and maintains commonly perceived stereotypes, in turn harming the self esteem of obese people. A charge of prejudice and/or discrimination on the basis of appearance could be leveled against these depictions.



Causes of Obesity
[edit | edit source]Conventional wisdom holds that obesity is caused by over-indulgence in fatty or sugary foods, portrayed as either a failure of will power or a species of addiction. Various specialists strongly oppose this view. For example, Professor Thomas Sanders, the director of the Nutrition, Food & Health Research Centre at King's College London, emphasises the need for balance between activity and consumption:
- In trials, there is no evidence suggesting that reducing fat intake has an effect on obesity. As long as your expenditure equals what you eat, you won't put on weight, regardless of how high the fat content is in your diet (The Times, London, 10 March 2004).
Obesity is generally a result of a combination of factors:
- Genetic predisposition
- Energy-rich diet
- Limited exercise and sedentary lifestyle
- Weight cycling, caused by repeated attempts to lose weight by dieting
- Underlying illness
- Certain eating disorders
- Poverty
Some eating disorders can lead to obesity, especially binge eating disorder (BED). As the name indicates, patients with this disorder are prone to overeat, often in binges. A proposed mechanism is that the eating serves to reduce anxiety, and some parallels with substance abuse can be drawn. An important additional factor is that BED patients often lack the ability to recognize hunger and satisfaction, something that is normally learned in childhood. Learning theory suggests that early childhood conceptions may lead to an association between food and a calm mental state.
While it is often quite obvious why a certain individual gets fat, it is far more difficult to understand why the average weight of certain societies have recently been growing. While genetic causes are central to who is obese, they cannot explain why one culture grows fatter than another. Although there is no definitive explanation for the recent epidemic of obesity, an evolutionary hypothesis offers one explanation. In times when food was scarce, the ability to take advantage of rare periods of abundance and use such abundance by storing energy efficiently was likely an evolutionary advantage. This is precisely the opposite of what is required in a sedentary society, where high-energy food is available in abundant quantities in the context of decreased exercise. Although many people may have a genetic propensity towards obesity, it is only with the reduction in physical activity and a move towards high-calorie diets of modern societies that it has become so widespread.
An alternative to an evolutionary hypothesis is an inequality hypothesis. In most developed nations, there are massive food surpluses, but these surpluses do not apply uniformly across populations. Similarly, sedentary lifestyles are not evenly distributed, and many of the populations experiencing increasing levels of obesity are rather active compared to other groups with lower levels of obesity. Even in the most developed nations, the people most likely to develop obesity tend to have the lowest access to quality foods and many of them spend considerable time being active due to work and/or family requirements. As a result, evolutionary hypotheses would suggest these people would take advantage of rare periods of abundance without developing obesity due to their lower levels of average consumption and moderate levels of activity. The opposite, however, is what occurs. Seeking to explain this phenomenon, researchers focused on neighborhood effects have systematically demonstrated that poverty is a more likely explanation for obesity. Specifically, people in impoverished areas often lack access to food available to more economically well off members of society, often only have access to foods that can lead to obesity (due to their high-calorie contents) within their neighborhoods (even if they maintain active lifestyles or working lives), and often lack access to many of the resources (e.g., stoves, cooking utensils, transportation to healthier grocery stores, electricity, etc.) necessary for taking advantage of food surpluses. While proponents of evolutionary hypotheses point to individualistic elements like exercise, genetics, diet selection, and sedentary lifestyles that suggest we may improve health without drastically altering our current economic, political, and health systems, proponents of social explanations (such as poverty and environmental pollution) note that even when researchers and advocates have found ways to minimize these individualistic elements (e.g., via food programs, dietary education protocols, exercise programs, limited or temporary economic support, and genetic interventions) the patterns of obesity have not changed much. As a result, these researchers hypothesize that obesity (and other health-related epidemics that have become common in the last couple hundred years) can only be understood (and thus combatted) by examining the social factors that may contribute to physiological, biological, genetic, and other health-related transformations, adaptations, and mutations within the bodies of people experiencing said social factors and shifts within our natural surroundings.[34][1][35]
As noted above, the obesity epidemic is most notable in the United States. In the years from just after the Second World War until 1960 the average person's weight increased, but few were obese. In 1960 almost the entire white population was well fed, but not overweight. In the two and a half decades since 1980 the growth in the rate of obesity has accelerated markedly (while mirroring the growth in poverty and food insecurity rates) and is increasingly becoming a public health concern. There are a number of theories as to the cause of this change since 1980, but most echo assumptions embedded within initial evolutionary hypotheses at present (and rely merely on assumptions that specific correlations are related to the fundamental cause of the issue), and thus may need to be readjusted in relation to emerging recognition of the limitations of these theories:
- Obese people appear to be less active in general than lean people, and not just because of their obesity. A controlled increase in calorie intake of lean people did not make them less active, nor, correspondingly, when obese people lost weight did they become more active. Weight change does not affect activity levels, but the converse seems to be the case.[36]
- Another important contributor to the current obesity concern is the much lower relative cost of foodstuffs: agricultural subsidies in the United States and Europe have led to lower food prices for consumers than at any other point in history.
- Marketing may also play a role. In the early 1980s the Reagan administration lifted most regulations for advertising to children. As a result, the number of commercials seen by the average child increased greatly, and a large proportion of these were for fast food and candy. There is now compelling evidence that children's exposure to food commercials on television increases the odds of childhood obesity.[37]
- Changes in the price of gasoline may also have had an effect, as unlike during the 1970s it is now affordable in the United States to drive everywhere, curtailing both foot traffic and the riding of bikes. An indication of the reliance on cars in the U.S. is the increasing number of areas that are built without sidewalks and parks.
- Increases in the service sector of the economy have resulted in a greater percentage of the population spending most of their workday behind a desk or computer.
- A social cause that is believed by many to play a role is the increasing number of two income households where one parent no longer remains home to look after the house. This increases the number of restaurant and take-out meals.
- Urban sprawl may also contribute to the increase in obesity rates, possibly due to less walking and less time for cooking.[38]
- Since 1980 both sit-in and fast food restaurants have seen dramatic growth in terms of the number of outlets and customers served. Low food costs and intense competition for market share led to increased portion sizes. For example, McDonalds' french fries portions rose from 200 calories in 1960 to over 600 calories today.
- Increasing affluence itself may be a cause or contributing factor since obesity tends to flourish as a disease of affluence in countries which are developing and becoming westernised (for more information on this factor, see here). This is supported by the observation of a dip in American GDP after 1990, the year of the Gulf War, followed by an exponential increase. U.S. obesity statistics followed the same pattern, offset by two years (source).
Some obesity co-factors are resistant to the theory that the epidemic is a new phenomenon. In particular, a class co-factor consistently appears across many studies. Comparing net worth with BMI scores, one study found obese American subjects were approximately half as wealthy as thin ones.[39] When income differentials were factored out, the inequity persisted: thin subjects were inheriting more wealth than fat ones. Another study finds women who married into a higher status were thinner than women who married into lower status. Like many other recent analyses of social patterning within obese and non-obese populations, these studies suggest that while evolutionary hypotheses provided an important starting point, the answers to the problems likely lie either elsewhere or via an integration of evolutionary and fundamental causes theories.[34]
Policy Responses to Obesity
[edit | edit source]On top of controversies about the causes of obesity, and about its precise health implications, come controversies about the correct policy approach to obesity. The main debate is between personal responsibility advocates, who resist regulatory attempts to intervene in citizen's private dietary habits, and public interest advocates, who promote regulations on the same public health grounds as the restrictions applied to tobacco products. Importantly, these suggestions are (thus far) primarily tied to evolutionary hypotheses, which suggests that they are more likely to influence individual cases and less likely to greatly effect the overall patterns. There is some evidence that the public interest approach may help, though it is clearly not the solution to the problem, and many activists worry that it will - like anti-smoking campaigns - ultimately become an attempt to limit the liberty and decision-making options for people rather than simply address the problems associated with consumption behaviors. A recent study found that parents order items for their children from fast food menus that total to just over 100 fewer calories when each item's calories are clearly labeled.[40] This suggests that raising awareness and educating consumers about the calorie content may help reduce the number of calories consumed for those individuals that have the privilege (e.g., the economic, social, and educational resources) to be selective in their and their children's dietary selections.
In the U.S., a recent bout in this controversy involves the so-called Cheeseburger Bill, an attempt to indemnify food industry businesses from frivolous law suits by obese clients. On July 16, 2004, the U.S. Department of Health and Human Services officially classified obesity as a disease. Speaking to a Senate committee, Tommy Thompson, the Secretary of Health and Human Services, stated that Medicare would cover obesity-related health problems. However, reimbursement would not be given if a treatment was not proven to be effective.
The Evolution of Health Care and Medicine
[edit | edit source]All human societies have beliefs that provide explanations for, and responses to, childbirth, death, and disease. Throughout the world, illness has often been attributed to witchcraft, demons, or the will of the gods, ideas that retain some power within certain cultures and communities (see faith healing). However, the rise of scientific medicine in the past two centuries has altered or replaced many historic health practices while granting others (regardless of their results at times) legitimacy in the public consciousness.
Folk Medicine
[edit | edit source]
Folk medicine refers collectively to procedures traditionally used for treatment of illness and injury, aid to childbirth, and maintenance of wellness. It is a body of knowledge distinct from modern, scientific medicine but may coexist in the same culture. It is usually unwritten and transmitted orally until someone collects it. Within a given culture, elements of folk medicine may be diffusely believed by many adults or may be gathered and applied by those in a specific role of healer, shaman, midwife, witch, or dealer in herbs. Elements in a specific culture are not necessarily integrated into a coherent system and may be contradictory. Folk medicine is sometimes associated with quackery when practiced as theatrics or otherwise practiced fraudulently, yet it may also preserve important cultural tradition from the past.
Herbal medicine is an aspect of folk medicine that involves the use of gathered plant parts to make teas, poultices, or powders that purportedly effect cures. Many effective treatments adopted by physicians over the centuries were derived from plants (e.g. aspirin), and botany was an important part of the materia medica of professional medical training before the 20th century. Attention has been paid to the folk medicine of indigenous peoples of remote areas of the world in the interest of finding new pharmaceuticals. Of concern is the extinction of many species by the clearing of formerly wild rainforests. Such activity may lead to the loss of species of plants that could provide aids to modern medicine. Attitudes toward this type of knowledge gathering and plant preservation vary and political conflicts have increasingly arisen over ownership of the plants, land, and knowledge in several parts of the world.
While potentially important as cultural tradition, folk medicine should not be considered a reliable or proven form of healthcare; anyone considering trying folk medicine should always consult with a scientifically trained doctor first while exploring ways that folk medicine may aid, enhance, or provide better options than scientifically based approaches (e.g., the herbs at the heart of aspirin use do not come with the same side-effects and potential blood and heart issues in later life that aspirin has).
Alternative Medicine
[edit | edit source]Alternative medicine describes methods and practices used in place of, or in addition to, conventional or scientific treatments. There is some debate as to what is included under the label "alternative," as these practices include things as far ranging as: spiritual, metaphysical, or religious treatments; Eastern and Asian traditional treatments; and a variety of unproven treatments, like acupuncture, chiropractic, healing-touch, and homeopathy. One popular definition of alternative medicine is provided by Richard Dawkins, an Oxford biologist: "that set of practices that cannot be tested, refuse to be tested or consistently fail tests."[41]
The widespread acceptance of various forms of alternative medicine is a good illustration of a combination of social-psychological ideas, including: fads, scientific illiteracy, the power of marketing in a capitalistic economy, the influence of misinformed politicians on public policy e.g., The National Center for Complementary and Alternative Medicine at the National Institutes of Health and the willingness of people without "alternatives" to turn to unproven therapies when modern medicine informs them there is nothing else that can be done. Importantly, these same processes often facilitate the practice of newfound scientific approaches to medicine before researchers know exactly what such treatments and pills may do to human beings over the life course.[42][43]
Western Medicine
[edit | edit source]
Healthcare improves as a result of some advancements in medical science. Western medicine approaches health care from two angles. The first, the medical model, focuses on the eradication of illness through diagnosis and effective treatment. The second, the social model, focuses on changes that can be made in society and in people's own lifestyles to make the population healthier. Western, scientific medicine has proven uniquely effective at treating and preventing some diseases while wholly inadequate in treating others. It is increasingly widespread and more widely accepted than other forms of medicine, but researchers cannot ascertain whether this is due to results, concerted political and economic campaigns to stigmatize other approaches, or some combination of both. Western medicine is notably secular in name, officially indifferent to ideas of the supernatural or the spirit, and officially concentrated on the body and society to determine causes and cures, but throughout history religious organizations and institutions (especially with corporate or economic backing) have exerted considerable influence upon much Western Scientific medical development and practice). Despite its issues and problem areas, most researchers believe that Western scientific medicine is the most effective contributor to the health of humans in the world today.
Criticisms of Alternative and Western Medicines
[edit | edit source]Some of the criticisms of alternative and western-science medicine include:
- Lack of Western Science approved testing. Many of the studies allegedly supporting the claims of alternative medicine are not controlled, double-blind peer-reviewed experiments, which is considered the gold standard in science and modern medicine (but they are also often not paid for and controlled by for-profit companies, which occurs throughout Western Scientific Medicine). The efficacy of these treatments has not been demonstrated through double-blind randomized controlled trials. Where alternative methods provide temporary symptomatic relief, this can usually be explained as being due to the placebo effect, to natural healing, or to the cyclical nature of some illnesses.
- Not proven to be an alternative. The term alternative medicine is misleading, as these treatments have not been proven to be an effective alternative to regulated conventional medicine, but alternative medicine proponents point out that the same can be said (not proven, though often demonstrated to be probable) of Western Medicine.
- Safety issues. Some alternative practices (like some Western medicine practices) have killed people.[44][45] While not all alternative medicine treatments are potentially lethal, many are, and as a result, Western Medical authorities argue that Western Scientific standards must be applied to these medicines in the same way they are applied to many Western Medicine treatments that are lethal (once again, even though not all are). The lack of oversight by government regulators like the Food and Drug Administration (similar to the lack of oversight it actually provides to the Western pharmaceutical industry[46]) allows those selling these products virtually free-reign to employ whatever techniques they can sell (similar to lessened marketing regulations concerning pharmaceutical sales). The result is a buyer beware situation in which consumers must discern whether the treatment is harmful regardless of whether such treatment comes from Alternative or Western medical traditions. Proponents of alternative medicine say that people should be free to choose whatever method of healthcare they want, and Western Medicine proponents make the same argument, but each group tends to highlight the benefits of their approach (for example, alternative approaches to birth and hemophilia) and western approaches to infectious disease and immune deficiency) without regard for their tradition's faults and controversies (for example, alternative approaches to pain relief that offered no herbal or pharmaceutical relief or western creation and treatment of diseases that likely did not exist - like hysteria, which was ultimately a response to gender inequality with little to no biological basis or consequence). Critics agree that people should be free to choose, but when choosing, people must be certain that whatever method they choose will be safe and effective. People who choose alternative or western medicines may think they are choosing a safe, effective medicine, while they may only be getting quack remedies. This issue is particularly important in the treatment of children and individuals whose capacity to evaluate the treatment is impaired.
- Delay in seeking conventional medical treatment. There is a concern that patients may delay seeking conventional medicine that could be more effective, while they undergo alternative therapies, potentially resulting in harm. At the same time, there is concern that patients often avoid alternative medicines that could be more effective due to the stigmatization of alternative approaches in Western societies. This is especially important - and part of the reason alternative and western approaches are being integrated in many settings - because human biology is incredibly complex, and often the answers to any condition require systematic comparison of multiple approaches and methods.
- Poor diagnosis. Western and Alternative doctors and practitioners hold that the other tradition sometimes fail to correctly diagnose illnesses and therefore does not provide safe therapies. With a minor illness this may not be a serious concern, but with more serious illness it can lead to injury, disfigurement, or death. In terms of alternative approaches, for example, the lack of vital monitoring practiced in some traditions may lead practitioners to miss important details concerning heart conditions, and in terms of western approaches, the emphasis on and history of dismissing women's concerns often leads to misdiagnosis of disorders due to focus upon the genital and reproductive organs.
- Cost. In countries where healthcare is state-funded or funded by medical insurance, alternative therapies are often not covered, and must be paid for by the patient. Costs for some therapies are relatively inexpensive, just several dollars for a medication. But others can be thousands of dollars and require continued payments for years and years.[44] Note, this is the same issue that faces the many people unable to acquire health insurance throughout the world.
- Issues of regulation. Neither alternative or western medicines are properly regulated.[46] As a result, there is often little to no governmental control on who practices alternative medicine and no real way of knowing what training or expertise they possess. In the United States, herbal remedies, vitamins, and supplements are not regulated by the Food and Drug Administration (FDA).[47][48] This means that companies are not required to prove that these supplements are either effective or safe. The failure to regulate supplements has led to serious health issues for some, including some deaths.[47] Such problems did ultimately lead the FDA to ban the sale of ephedra. Similarly, there is often little to no governmental control over pharmaceutical research and practices, and much pharmaceutical (and other Western) medical research is subsidized by corporations in search of profits rather than health, which leaves patients with no real way of knowing whether or not their "medicine" is actually a good idea or simply an addition to the bottom line. A notable example of this problem can be seen in western medical science approaches to breast cancer where - especially since the 1980's - corporate profits from the condition have exploded while treatment remains relatively the same as the 1940's approach (e.g., burn, slash and kill), where mammograms - supported by science funded by companies that create and sell mammography machines - and detection have become the focus to the detriment of attempts to compel researchers to search for cures and new treatment protocols, where billions of dollars are raised each year for research without any accountability concerning where this money goes, and where the most scientific answers to the problem itself (e.g., environmental factors that mirror rates of breast cancer in society since the 1930's) are completely ignored, unfunded, and left to private researchers to study.[49] Considering the amount of people that die each year from breast cancer related conditions or issues, the lack of oversight (and scientific ethics) in much of the Western Medical tradition (similar to alternative traditions) is quite astounding and powerful in its consequences.
- Testing and studies. The western scientific community argues that many studies carried out by alternative medicine promoters are flawed, as they often use testimonials and hearsay as evidence, leaving the results open to observer bias. They argue that the only way to counter observer bias is to run a double-blind experiment in which neither the patient nor the practitioner knows whether the real treatment is being given or if a placebo has been administered. This research should then be reviewed by peers to determine the validity of the research methodology. Testimonials are particularly disturbing in this regard because, by chance alone, some people may see some improvement in the ailment for which they are being treated and will proceed to testify that the method helped them when the method was not the true cause of improvement.[50] Interestingly, promoters of Alternative Medicine levy the exact same complaint at the foot of western medical science - due to the pharmaceutical funding and oversight of most western "experiments", the studies are automatically victims of observer bias in their construction in much the same way western scientists argue alternative medicine may be biased in their procedures. For example, much breast cancer research and treatment science is funded by and subject to the funding of cosmetic companies that incidentally offer the products most highly correlated with breast cancer in America today (e.g., it is like having tobacco companies manage the scientific study of smoking - for a useful took where you can examine the cancer-causing content of your cosmetics see the recommended reading at the end of this section).[51] Analyses across both fields often finds similar problematic procedures in both fields, but recent attempts to integrate (rather than demonize) these fields may be capable of reducing these problems.[51]
Recognizing the complexity of these issues, it is important for all people to learn about various aspects of health and well being, methods of critical thinking and decision making, and ways to keep abreast of ongoing developments within and between western-science and alternative medical traditions, practices, problems, benefits, and limitations. In so doing, people may ascertain the best health-related practices for themselves and the people they care about while also pushing both of these medical traditions toward greater regulation, oversight, integration, and care practices for all people.
Additional Reading
[edit | edit source]- The New York Times recently invited a professor of bioethics to discuss the ethics of rationing healthcare. This article would serve as a very good launching point for discussing the ethics of universal healthcare. http://www.nytimes.com/2009/07/19/magazine/19healthcare-t.html
- At this website, you may read the entire Affordable Care Act, or use the tabs to find the information most useful to you. Of particular interest are the timeline and the Key Features for the law, as well as the young adult section of the website (young adult defined as anyone under the age of 26) because it will probably have most of the changes that will directly effect most college students. Keep in mind this is the official site for the law, which means two important things: (1) it is constantly checked for accuracy by researchers so you will be getting the proper information about the law and changes, and (2) it is regularly updated as new developments, decisions, or time marks pass during the roll out of the law. http://www.healthcare.gov/law/index.html
Further examples
Rosich, Katherine and Janet Hankin. 2010. “Executive Summary: What Do We Know? Key Findings from 50 Years of Medical Sociology.” Journal of Health and Social Behavior, Extra Issue, 51:S1-S9.
Burdette, Amy and Terrence Hill. 2008. “An examination of processes linking perceived neighborhood disorder and obesity.” Social Science & Medicine 67:38-46.
Ross, Catherine and John Mirowsky. 2000. “Does Medical Insurance Contribute to Socioeconomic Differentials in Health?” The Milbank Quarterly 78:291−321.
Busfield, Joan. 2006. “Pills, Power, People: Sociological Understandings of the Pharmaceutical Industry.” Sociology 40(2):297-314.
Rier, David A. 2000. “The missing voice of the critically ill: a medical sociologist’s firstperson account.” Sociology of Health & Illness 22(1):68-93.
Smith, Allen and Sherryl Kleinman. 1989. “Managing Emotions in Medical School.” Social Psychology Quarterly, 52:6-69.
Chrisler, Joan and Paula Caplan. 2002. “The Strange Case of Dr. Jekyll and Ms. Hyde: How PMS became a Cultural Phenomenon and Psychiatric Disorder.” Annual Review of Sex Research 13:274-306.
““But we have to do Something”: Surgical Correction of Atypical Genitalia.” by Katrina Roen
Akers, Aletha Y., Melvin R. Muhammad, and Giselle Corbie-Smith. 2011. “‘When you got nothing to do, you do somebody’: A community’s perceptions of neighborhood effects on adolescent sexual behaviors.” Social Science & Medicine 72:91-99.
Winterich, Julie A. 2003. Sex, Menopause, and Culture: Sexual Orientation and the Meaning of Menopause for Women’s Sex Lives. Gender & Society 17(4): 627-642.
Elson, Jean. 2003. Hormonal Hierarchy: Hysterectomy and Stratified Stigma. Gender & Society 17(5): 750-770.
Brubaker, Sarah Jane. 2007. Denied, Embracing, and Resisting Medicalization: African American Teen Mothers’ Perceptions of Formal Pregnancy and Childbirth Care. Gender & Society 21(4): 528-552.
Kelly, Kimberly, and Linda Grant. 2007. State Abortion and Nonmarital Birthrates in the Post-Welfare Reform Era: The Impact of Economic Incentives on Reproductive Behaviors of Teenage and Adult Women. Gender & Society 21(6): 878-904.
Discussion Questions
[edit | edit source]- What does it mean to be healthy?
- Would you prefer private or public health care?
- What do you think is contributing to the prevalence of obesity in many countries?
- How long have we had science-based medical treatments?
References
[edit | edit source]- ↑ a b Rosich, Katherine and Janet Hankin. 2010. “Executive Summary: What Do We Know? Key Findings from 50 Years of Medical Sociology.” Journal of Health and Social Behavior, Extra Issue, 51:S1-S9.
- ↑ a b Simon, Stephanie, and Betsy McKay. 2009. “Developing World's Parasites, Disease Hit U.S..” wsj.com, August 22 http://online.wsj.com/article/SB125090339313750961.html (Accessed August 24, 2009).
- ↑ Burdette, Amy M. and Belinda L. Needham. 2012. “Neighborhood Environment and BMI Trajectories from Adolescence to Adulthood” Journal of Adolescent Health 50: 30-37.
- ↑ Burdette, Amy M. Terrence D. Hill and Lauren Hale. 2012. “Household Disrepair and the Mental Health of Low-income Urban Women.” Journal of Urban Health: Bulletin of the New York Academy of Medicine 88: 142-153.
- ↑ Hale, Lauren, Terrence D. Hill and Amy M. Burdette. 2010. “Sleep Quality as a Mediator of Neighborhood Effects on Health” Preventive Medicine 51: 275-278
- ↑ Hill, Terrence D., Amy M. Burdette, and Lauren Hale. 2009. “Neighborhood Disorder, Sleep Quality, and Psychological Distress: A Model of Structural Amplification” Health and Place 15: 1006- 1013
- ↑ Rieker, Patricia, Chloe Bird, and Martha Lang. 2013. “Understanding Gender and Health: Old Patterns, New Trends, and Future Directions.” Pp. 52−74 in Handbook of Medical Sociology, 6th Edition, edited by C. Bird, P. Conrad, A. Fremont, and S. Timmermans. Nashville, TN: Vanderbilt University Press.
- ↑ John Dececco Phd, Michael Scarce. 1999. Smearing the Queer: Medical Bias in the Health Care of Gay Men. Routledge.
- ↑ a b Goldberg, Lisa, Ami Harbin, and Sue Campbell. 2011. “Queering the Birthing Space: Phenomenological Interpretations of the Relationships between Lesbian Couples and Perinatal Nurses in the Context of Birthing Care.” Sexualities 14(2):173–92.
- ↑ Chrisler, Joan and Paula Caplan. 2002. “The Strange Case of Dr. Jekyll and Ms. Hyde: How PMS became a Cultural Phenomenon and Psychiatric Disorder.” Annual Review of Sex Research 13:274-306.
- ↑ Katz, Jonathan Ned. 2007. The Invention of Heterosexuality. University of Chicago Press.
- ↑ Wodtke, Geoffrey T. et al, Concentrated poverty, ambient air pollution, and child cognitive development, Science Advances (2022). DOI: 10.1126/sciadv.add0285
- ↑ Williams, Brie A., Karla Lindquist, Rebecca L. Sudore, Kenneth E. Covinsky, and Louise C. Walter. 2008. “Screening Mammography in Older Women: Effect of Wealth and Prognosis.” Arch Intern Med 168:514-520.
- ↑ a b c d e f Pear, Robert. 2008. “Gap in Life Expectancy Widens for the Nation.” The New York Times, March 23 http://www.nytimes.com/2008/03/23/us/23health.html (Accessed March 25, 2008).
- ↑ Wen M, Browning CR & Cagney K. 2007. “A multi-level study of neighborhood environment and its relationship to physical activity in adulthood” Urban Studies:44(13): 1-18.
- ↑ Akers, Aletha Y., Melvin R. Muhammad, and Giselle Corbie-Smith. 2011. “‘When you got nothing to do, you do somebody’: A community’s perceptions of neighborhood effects on adolescent sexual behaviors.” Social Science & Medicine 72:91-99.
- ↑ Borkhoff, Cornelia M. et al. 2008. “The effect of patients' sex on physicians' recommendations for total knee arthroplasty.” CMAJ 178:681-687.
- ↑ Giuffre, Patti A., and Christine L. Williams. 2000. “NOT JUST BODIES Strategies for Desexualizing the Physical Examination of Patients.” Gender & Society 14(3):457–82.
- ↑ a b Griffith, D.M., Allen, J.O. & Gunter, K. (2010). Social and Cultural Factors Influence African American Men’s Medical Help-seeking. Research on Social Work Practice. Published online 18 November 2010. Special issue on African American males.
- ↑ Adimora, Adaora A., Victor J. Schoenbach, and Michelle A. Floris-Moore. 2009. “Ending the Epidemic of Heterosexual HIV Transmission Among African Americans.” American Journal of Preventive Medicine 37:468-471.
- ↑ Lane, Sandra D. et al. 2004. “Structural Violence and Racial Disparity in HIV Transmission.” Journal of Health Care for the Poor and Underserved 15(3):319–35.
- ↑ Ross, Catherine and John Mirowsky. 2000. “Does Medical Insurance Contribute to Socioeconomic Differentials in Health?” The Milbank Quarterly 78:291−321.
- ↑ a b Banks, James; Marmot, Michael; Oldfield, Zoe, and Smith, James P. Disease and Disadvantage in the United States and in England. JAMA. 2006 May 3; 295(17):2037-2045
- ↑ Willson, Andrea E. 2009. “'Fundamental Causes' of Health Disparities: A Comparative Analysis of Canada and the United States.” International Sociology 24:93-113.
- ↑ Schoen, Cathy, Robin Osborn, Sabrina K.H. How, Michelle M. Doty, and Jordon Peugh. 2009. “In Chronic Condition: Experiences Of Patients With Complex Health Care Needs, In Eight Countries, 2008.” Health Aff 28:w1-16.
- ↑ Wennberg, John E., Elliott S. Fisher, David C. Goodman, Jonathan S. Skinner, and Sandra M. Sharp. 2008. Tracking the Care of Patients with Severe Chronic Illness: The Dartmouth Atlas of Health Care 2008. Lebanon, New Hampshire: The Dartmouth Institute for Health Policy & Clinical Practice http://web.archive.org/web/20090325003539/http://www.dartmouthatlas.org/atlases/2008_Chronic_Care_Atlas.pdf (Accessed April 13, 2008).
- ↑ Krugman, Paul. 2008. “Health Care Horror Stories.” The New York Times, April 11 http://www.nytimes.com/2008/04/11/opinion/11krugman.html (Accessed April 13, 2008).
- ↑ Kolata, Gina. 2008. “Co-Payments Soar for Drugs With High Prices.” The New York Times, April 14 http://www.nytimes.com/2008/04/14/us/14drug.html (Accessed February 11, 2010).
- ↑ Toner, R., & Elder, J. (2007). Most Support U.S. Guarantee of Health Care. The New York Times. Retrieved March 2, 2007, from http://www.nytimes.com/2007/03/02/washington/02poll.html
- ↑ Strully, K. W. (2009). “Job Loss and Health in the U.S. Labor Market.” Demography 46(2):
- ↑ Rimm, E B, P Williams, K Fosher, M Criqui, and M J Stampfer. 1999. “Moderate alcohol intake and lower risk of coronary heart disease: meta-analysis of effects on lipids and haemostatic factors.” BMJ (Clinical Research Ed.) 319:1523-1528.
- ↑ Abdulla, S. 1997. “Is alcohol really good for you?.” Journal of the Royal Society of Medicine 90:651.
- ↑ Swami, Viren, Natalie Salem, Adrian Furnham, and Martin J. Tovee. 2008. “The influence of feminist ascription on judgements of women's physical attractiveness.” Body Image.
- ↑ a b Link, Bruce G. and Jo Phelan. 2010. “Social Conditions as Fundamental Causes of Health Inequalities.” Pp. 3−17 in Handbook of Medical Sociology, 6th Edition, edited by C. Bird, P. Conrad, A. Fremont, and S. Timmermans. Nashville, TN: Vanderbilt University Press.
- ↑ Burdette, Amy and Terrence Hill. 2008. “An examination of processes linking perceived neighborhood disorder and obesity.” Social Science & Medicine 67:38-46.
- ↑ Levine JA, Lanningham-Foster LM, McCrady SK, Krizan AC, Olson LR, Kane PH, Jensen MD, Clark MM. Interindividual variation in posture allocation: possible role in human obesity. Science 2005;307:584-6. PMID 15681386.
- ↑ Zimmerman, Frederick J., and Janice F. Bell. 2010. “Associations of Television Content Type and Obesity in Children.” Am J Public Health 100:334-340.
- ↑ Lopez R. Urban sprawl and risk for being overweight or obese. Am J Publ Health 2004;94:1574-9. PMID 15333317.
- ↑ Zagorsky, Jay L. 2005. “Health and Wealth. The Late-20th Century Obesity Epidemic in the U.S.” Economics and Human Biology 3(2):296–313.
- ↑ Tandon, Pooja S., Jeffrey Wright, Chuan Zhou, Cara Beth Rogers, and Dimitri A. Christakis. 2010. “Nutrition Menu Labeling May Lead to Lower-Calorie Restaurant Meal Choices for Children.” Pediatrics peds.2009-1117.
- ↑ Dawkins, Richard in Snake Oil, and Other Preoccupations by John Diamond. 2003. http://www.simonyi.ox.ac.uk/dawkins/writings/snakeoil.shtml
- ↑ Tiefer, Lenore. 2006. “The Viagra Phenomenon.” Sexualities 9:273-294.
- ↑ Busfield, Joan. 2006. “Pills, Power, People: Sociological Understandings of the Pharmaceutical Industry.” Sociology 40(2):297-314.
- ↑ a b Willmsen, Christine, and Michael J. Berens. 2007. “Public never warned about dangerous device.” The Seattle Times, November 19 http://seattletimes.nwsource.com/html/localnews/2004022178_miracle19m2.html (Accessed April 13, 2008).
- ↑ Imrie, Robert. 2008. “Parents Pick Prayer Over Doctor, Girl Dies.” AOL News, March 28 http://news.aol.com/health/story/ar/_a/parents-pick-prayer-over-doctor-girl/20080327161309990002 (Accessed April 13, 2008).
- ↑ a b Busfield, Joan. 2006. “Pills, Power, People: Sociological Understandings of the Pharmaceutical Industry.” Sociology 40(2):297-314.
- ↑ a b Brody, Jane E. 2008. “Potential for Harm in Dietary Supplements.” The New York Times, April 8 http://www.nytimes.com/2008/04/08/health/08brod.html (Accessed April 13, 2008).
- ↑ “Memory Supplements Forgettable, Says CSPI.” http://www.cspinet.org/new/200705041.html (Accessed April 13, 2008).
- ↑ Sulik, Gayle. 2012. Pink Ribbon Blues: How Breast Cancer Culture Undermines Women's Health. Oxford University Press.
- ↑ Beyerstein, Barry L. n.d. “Why Bogus Therapies Often Seem to Work.” quackwatch.org. http://www.quackwatch.org/01QuackeryRelatedTopics/altbelief.html (Accessed April 13, 2008).
- ↑ a b Sulik, Gayle. 2012. Pink Ribbon Blues: How Breast Cancer Culture Undermines Women's Health. Oxford University Press.
External links
[edit | edit source]- The Guardian has an excellent graphic illustrating leading causes of death by age, sex, and region of the world in 1900 and 2010.
- The Scientific Review of Alternative Medicine
- International health statistics comparison
- International Health Statistics: What the Numbers Mean for the United States - 1994
- Joint CDC/StatsCan comparison on the two health care systems - 2004 (pdf)
- Fetal Alcohol Syndrome Diagnostic & Prevention Network (FAS DPN)
- Well.com FAS Fact Sheet
- FAQ on FAS from National Organization on Fetal Alcohol Syndrome
- Dr Sterling Clarren's keynote address on FASD, Prairie Northern Conference on Fetal Alcohol Syndrome, Yukon 2002
- Moderate alcohol intake and lower risk of coronary heart disease: meta-analysis of effects on lipids and haemostatic factors
- National Center on Minority Health and Health Disparities
- Understanding Health Disparities
- Initiative to Eliminate Racial and Ethnic Disparities in Health United States government minority health initiative
- Health Disparities Collaborative
- American Public Health Association. "Eliminating Health Disparities: Toolkit" (2004)
- Obesity, BMI and Calorie assessment Calculators
- Body Mass Index Calculator
- Obesity advice / FAQs
- International Task Force on Obesity
- Childhood Obesity
- Argument that the concern for obesity is overwrought
- BMJ Article on Obesity and Public policy
- Economics of Obesity
- The Worldwide Obesity Epidemic by Frank Sacks MD
- Infographic on healthcare costs in the US.
- inspiredhealthgroup.com
- goodhealthnevada.com
- This website provides information that allows people to ask questions and find answers concerning medical topics. It is continuously updated and regulated by staff at Columbia University. http://goaskalice.columbia.edu/
- This is a resource site for educational materials about contraceptive and reproductive health options http://bedsider.org/
- This site provides information on the content and potential health problems (especially breast cancer) associated with cosmetic brands. http://www.ewg.org/skindeep/
- Index Mundi lets you build current-to-the-year trend graphs for a wide variety of different topics. You can also compare across many different nations. http://www.indexmundi.com/facts/topics/health
- Behavioral Risk Factor Surveillance System (BRFSS) has reports and graphs, maps, etc. for many health-related topics. http://www.cdc.gov/brfss/
- National Center for Health Statistics (NCHS), another CDC resource provides statistics on a variety of health-related topics. http://www.cdc.gov/nchs/
- For those interested in FL specifically, there is the ever-expanding Florida CHARTS. http://www.floridacharts.com/charts/default.aspx
