Fundamentals of Human Nutrition/Vitamin D
7.2 Vitamin D
[edit | edit source]Introduction
[edit | edit source]- Vitamin D has been traditionally known as anti-ricketic factor or sunshine vitamin.
- Vitamin D is unique because it is a vitamin synthesized by the body and it functions as a hormone.
- Besides its pivotal role in calcium homeostasis and bone mineral metabolism, vitamin D endocrine system in now recognized to sub-serve a wide range of fundamental biological functions in cell differentiation, inhibition of cell growth as well as immunomodulation.
- It is a steroid that regulates complex system of genomic functions and has a role in prevention of neo plastic transformation.
- Recent evidences from genetic, nutritional and epidemiological studies link vitamin D endocrine system with diseases like hypertension, myopathic disorders, and proneness to infection, autoimmune disorders and cancer.
- Vitamin D modulates the transcription of cell cycle proteins which decrease cell proliferation and increase cell differentiation of a number of specialized cells of the body (osteoclastic precursors, enterocytes, keratinocytes.[1]
Vitamin D is not an essential nutrient, even though it is considered a vitamin, it is more of a hormone. Vitamin D needs to be activated in order for it to function. This can be done one of two ways either by UV radiation from the sun or through consumption of foods. Given a good amount of time in the sun, vitamin D can be synthesized without it being directly derived from food (Whitney 11.2). This process of synthesizing vitamin D from the sun can be seen in the epigenetics of humans. Since Paleolithic time, there has been potential change in vitamin D. During this era, people lived outside and did not wear any clothing to block their skin from the sun. So what exactly is the difference between the amount of sunlight we received before compared to now? Sun exposure is a necessary factor to activate the vitamin D cholesterol but the exact amount of UV sunlight that is necessary is not clear. It is said that five to fifteen minutes of sun exposure three times a week to the face, arms, legs, or back may be all that is needed to absorb a suitable amount of vitamin D (Cleveland Clinic Health Fact Sheet). Factors that may affect the amount of sunlight necessary include age, skin color, and location. Older people, dark skinned people and those living in northern climates might need more sun exposure (Cleveland Clinic Health Fact Sheet).
7.2.1 Source
[edit | edit source]Vitamin D can be found in a small handful of foods such as:
- Oily fish (salmon, sardines, mackerel, tuna)
- Eggs
- Powdered milk
- Breakfast cereals
- Fortified fat spreads (margarine)
- cheese
Concentrated food sources of vitamin D include sardines, cow's milk, goat's milk, shiitake mushrooms, and eggs. Among salmon, wild-caught fish have been shown to average significantly more vitamin D than non-organically farmed fish.[2]
As well as food, you can get vitamin D from sunlight, due to a reaction under the skin between ultraviolet light in sunlight and chemicals in the body.
The term "vitamin D" refers to several different forms of this vitamin. Two forms are important in humans: ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3). Vitamin D2 is synthesized by plants. Vitamin D3 is synthesized by humans in the skin when it is exposed to ultraviolet B (UVB) rays from sunlight. Foods may be fortified with vitamin D2 or D3.
Forms of Vitamin D
The two major forms are vitamin D2 or ergocalciferol, and vitamin D3 or cholecalciferol; vitamin D without a subscript refers to either D2 or D3 or both. These are known collectively as calciferol.[8] Vitamin D2 was chemically characterized in 1931. In 1935, the chemical structure of vitamin D3 was established and proven to result from the ultraviolet irradiation of 7-dehydrocholesterol.(9)
Name Chemical composition Structure
Vitamin D1 molecular compound of ergocalciferol with lumisterol, 1:1
Vitamin D2 ergocalciferol (made from ergosterol)
Vitamin D3 cholecalciferol (made from 7-dehydrocholesterol in the skin).
Vitamin D4 22-dihydroergocalciferol
Vitamin D5 sitocalciferol (made from 7-dehydrositosterol)
7.2.2 Functions
[edit | edit source]The main function of vitamin D in our body is that it promotes the use and absorptions of calcium and phosphate in the stomach so that healthy bones and teeth are maintained. Other roles of vitamin d are for cell growth and for the reduction of inflammation in the body.
- Help optimize calcium metabolism
- Help optimize phosphorus metabolism
- Help prevent type 2 diabetes, insulin resistance, high blood pressure, heart attack, congestive heart failure, and stroke
- Help prevent falls and muscle weakness
- Help prevent osteoporosis while maintaining bone integrity
- Help regulate insulin activity and blood sugar balance
- Help regulate immune system responses
- Help regulate muscle composition and muscle function
- Help regulate blood pressure
- Lower risk of excessive inflammation
- Lower risk of some bacterial infections
- Support cognitive function, especially in older persons
- Support mood stability, especially in older persons
- Help prevent chronic fatigue
- Help prevent the following types of cancer: bladder, breast, colon, ovarian, prostate and rectal
Reference • http://www.nutristrategy.com/nutrition/vitamind.htm
- http://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
- http://www.whfoods.com/genpage.php?tname=nutrient&dbid=110
Production in the skin
n the epidermal strata of the skin, production is greatest in the stratum basale and stratum spinosum.
Vitamin D3 (cholecalciferol) is produced photochemically in the skin from 7-Dehydrocholesterol . 7-Dehydrocholesterol is produced in relatively large quantities, 10,000 to 20,000 IU of vitamin D are produced in 30 minutes of whole-body exposure, in the skin of most vertebrate animals, including humans.(10)
7-dehydrocholesterol reacts with ultraviolet light of UVB type at wavelengths between 270 and 300 nm, with peak synthesis occurring between 295 and 297 nm.[11] These wavelengths are present in sunlight when the UV index is greater than three, as well as in the light emitted by the UV lamps in tanning beds (which produce ultraviolet primarily in the UVA spectrum, but typically produce 4% to 10% of the total UV emissions as UVB). At a UV index greater than three, which occurs daily within the tropics, daily during the spring and summer seasons in temperate regions, and almost never within the arctic circles, vitamin D3 can be made in the skin. Even if the UV index is high enough, exposure to light through windows is insufficient because UV light cannot pass through windows.[12]
Depending on the intensity of UVB rays and the minutes of exposure, an equilibrium can develop in the skin, and vitamin D degrades as fast as it is generated.[13]
The skin consists of two primary layers: the inner layer called the dermis, composed largely of connective tissue, and the outer, thinner epidermis. Thick epidermis in the soles and palms consists of five strata; from outer to inner they are: the stratum corneum, stratum lucidum, stratum granulosum, stratum spinosum, and stratum basale. Vitamin D is produced in the two innermost strata, the stratum basale and stratum spinosum.
The naked mole rat appears to be naturally cholecalciferol deficient, as serum 25-OH vitamin D levels are undetectable.[14] In some animals, the presence of fur or feathers blocks the UV rays from reaching the skin. In birds and fur-bearing mammals, vitamin D is generated from the oily secretions of the skin deposited onto the feathers or fur and is obtained orally during grooming.[15]
The Role of Vitamin D in our body:
Vitamin D is known as a vitamin however it is actually a hormone when it is in its active form. Vitamin D contains a binding protein that transports it to the vital organs necessary, which are mainly the bones, kidneys and intestines (Whitney & Rolfes, 2013). One of the major roles of Vitamin D in our body is bone health, specifically its’ assistance in the absorption of calcium and phosphorous and their blood concentrations. As these minerals are absorbed and deposited the bones in our body gradually strengthen and gain density that is vital for bone health. According to the text by Whitney in 2013, a Vitamin D sufficient diet promotes absorption from the GI tract, but Vitamin D also acts in an insufficient diet by providing the necessary minerals from other places like the kidneys and through mobilization from bones. Based on many studies, in addition to bone health, Vitamin D is also vital in preventing and treating “diabetes, heart disease, high blood pressure, and multiple sclerosis” (Cleveland Clinic, 2015). Vitamin D is also found to be helpful in preventing breast cancer, colon and prostate cancers. Vitamin D is equally important in regulating the immune and neuromuscular systems (DeNoon).
Vitamin D can help prevent type II diabetes which is a condition in which the body collects sugar in the blood stream. Type II diabetes typically develops after the age of 40, but can also develop sooner. Vitamin D and its role in regulating calcium can help control sugar in the blood. The pancreatic beta cells in the pancreas that produces insulin does not work well for individuals with type II diabetes. Research has shown that there are receptors in the beta cells that can only be activated by vitamin D. Therefore, it is hypothesized that vitamin D can help improve the production of insulin that allows the body to turn sugar into glucose. Furthermore, calcium helps regulate the release of insulin. Hence, sufficient levels of vitamin D increases the bioavailability of calcium, which in turn aids the emission of insulin (Chiu, 2004). Vitamin D also helps prevent heart diseases and heart failures. Coronary heart disease occurs when blood supply to the heart is blocked and congestive heart failure is when the heart cannot pump adequate amount of blood to the body. In both cases, high levels of vitamin D can reduce the chances of cardiovascular disease. This is due to the fact that vitamin D lowers diabetes (as explained above) and high blood pressure. Vitamin D can also help reduce thickening of artery walls and respiratory infections and inflammations (Anderson, 2010).
Vitamin D also acts with our skin cells using sunlight. This occurs when specific wavelengths of ultraviolet B light from the sun attach to our skin cells, 7-dehydrocholesterol, a molecule in our skin cells, can be converted into the initial form of vitamin D called cholecalciferol (The World's Healthiest Foods). There are countless things that could effect vitamin D production so it would be hard to tell exactly how much Vitamin D can be produced though the interaction of our skin cells and sunlight. Vitamin D is also vital in the body’s immunity because it is active in the maturation of white blood cells, which assist the body in defending itself from infections. Based on recent research studies have found that respiratory infections show connections with low vitamin D (The World's Healthiest Foods). As we age, our bones get weaker over time, and many elderly individuals suffer from things like osteoporosis, bone loss and overall weakness of their muscles and this is because it is more challenging to activate Vitamin D with age. Vitamin D can also be beneficial for the activity of genes that regulate cell growth, which in turn can be useful in treating diseases such as “metabolic syndrome, type 2 diabetes, tuberculosis, inflammation, multiple sclerosis, macular degeneration, hypertension, and some cancers” (Whitney & Rolfes, 2013). The Vitamin D hormone allows osteoblasts to produce a specific ligand, which then stimulates osteoclastogenesis that allows for bone resorption. Because of this the vitamin D plays a very vital role in “allowing individuals to mobilize calcium from bone when it is absent from the diet” (DeLuca, 2004). In summary Vitamin D has several functions, the most vital being its roles in bone healthy, immunity, skin, blood sugar, and its prevention of numerous diseases.
References
[edit | edit source]- ↑ Harinarayanan, C., & Shashank, R. J. (2009). Vitamin d status in india – its implications and remedial measures. In C. JAPI (Ed.), JAPI-review article (Vol. 57, pp. 40-49). India: JAPI. doi:www.japi.org
- ↑ http://www.whfoods.com/genpage.php?tname=nutrient&dbid=110
- DeLuca, H. (2004). Overview of general physiologic features and functions of vitamin D1,2,3,4. The American Journal of Clinical Nutrition. Retrieved December 1, 2015, from http://ajcn.nutrition.org/content/80/6/1689S.full
- DeNoon, J. Daniel (n.d.). Vitamin D FAQ: Why You Need Vitamin D. Retrieved December 1, 2015, from http://www.webmd.com/osteoporosis/features/the-truth-about-vitamin-d-why-you-need-vitamin-d
- The Role Of Vitamin D In Your Health. (2015). Retrieved December 1, 2015, fromhttps://my.clevelandclinic.org/health/diseases_conditions/hic_Osteoporosis/hic_The_role_of_vitamin_D_in_your_health
- The World's Healthiest Foods. (n.d.). Vitamin D. Retrieved 2015, from http://www.whfoods.com/genpage.php?tname=nutrient&dbid=110#function
- Whitney, E., & Rolfes, S. (2013). Understanding Nutrition (14th ed.). Belmont, CA: Cengage Learning.
Mechanism of action
[edit | edit source]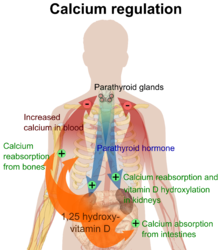
Vitamin D is carried in the bloodstream to the liver, where it is converted into the prohormone calcidiol. Circulating calcidiol may then be converted into calcitriol, the biologically active form of vitamin D, either in the kidneys or by monocyte- macrophages in the immune system. When synthesized by monocyte-macrophages, calcitriol acts locally as a cytokine, defending the body against microbial invaders.[16][2] Following the final converting step in the kidney, calcitriol (the physiologically active form of vitamin D) is released into the circulation. By binding to vitamin D-binding protein (VDBP), a carrier protein in the plasma, calcitriol is transported to various target organs.[3]
Calcitriol mediates its biological effects by binding to the vitamin D receptor (VDR), which is principally located in the nuclei of target cells.[3] The binding of calcitriol to the VDR allows the VDR to act as a transcription factor that modulates the gene expression of transport proteins (such as TRPV6 and calbindin), which are involved in calcium absorption in the intestine.[17][4] The vitamin D receptor belongs to the nuclear receptor superfamily of steroid/thyroid hormone receptors, and VDRs are expressed by cells in most organs, including the brain, heart, skin, gonads, prostate, and breast. VDR activation in the intestine, bone, kidney, and parathyroid gland cells leads to the maintenance of calcium and phosphorus levels in the blood (with the assistance of parathyroid hormone and calcitonin) and to the maintenance of bone content.[18]([5]) Vitamin D increases expression of the hydroxylase gene in adrenal medullary cells. It also is involved in the biosynthesis of neurotrophic factors, synthesis of nitric oxide synthase, and increased glutathione levels.[19]([6])
The VDR is known to be involved in cell proliferation and differentiation. Vitamin D also affects the immune system, and VDRs are expressed in several white blood cells, including monocytes and activated T cell and B cells.[20]([7])
Apart from VDR activation, various alternative mechanisms of action are known. An important one of these is its role as a natural inhibitor of signal transduction by hedgehog (a hormone involved in morphogenesis).[21][22]([8])[9]
One of the most important roles of vitamin D is to maintain skeletal calcium balance by promoting calcium absorption in the intestines, promoting bone resorption by increasing osteoclast number, maintaining calcium and phosphate levels for bone formation, and allowing proper functioning of parathyroid hormone to maintain serum calcium levels. Vitamin D deficiency can result in lower bone mineral density and an increased risk of reduced bone density (osteoporosis) or bone fracture because a lack of vitamin D alters mineral metabolism in the body.[23]([10]) Thus, although it may initially appear paradoxical, vitamin D is critical for proper bone formation despite its role as a potent stimulator of bone resorption.[24]([11])
7.2.3 Requirements
[edit | edit source]The recommended daily allowance of vitamin d for adults over 50 years is 400-800 i.u. For people aged 25–50 years the recommended daily allowance of vitamin D is 400 i.u. In order to maintain a healthy level of vitamin d you need consume the sorts of food that contain it such as fatty fish, eggs, milk and cereal. Also by exposing your body to the sunlight for 15 minutes for 2–3 days a week you can make your body satisfied on the amount of vitamin d you have consumed through the skin.
CHANGING DEFINITIONS OF VITAMIN D STATUS
Based on the study of bio markers like PTH and intestinal calcium absorption and functional health outcomes, there has been a dramatic change in the definition of vitamin D deficiency over last few years. Institute of Medicine and the American Academy of Paediatrics (AAP) in 1997 defined vitamin D deficiency in infants and children as a serum 25 (OH) D level below 11 ng/mL[12] but level below 20 ng/mL are now considered insufficient [4]. Table I shows the classification of vitamin D status based on serum 25 (OH) D level [4]. IOM recently published a review [13] on dietary reference intakes for calcium and vitamin D. This review expressed that, as studies regarding non-skeletal health benefits provided mixed and inconclusive results, as yet there is insufficient evidence to recommend higher levels of serum 25(OH)D. It feels that benefits for most in the population is associated with levels of approximately 20 ng/ml and use of higher cut-off s would artificially increase the estimates of prevalence of vitamin D deficiency. This review has taken skeletal health as the basis for Dietary Reference Intakes (DRI). There is an urgent need to follow these current definitions of vitamin D status, as paediatricians (and obstetricians) are blamed for being a little slow to address the suboptimal vitamin D status of their patients.
| Vitamin D status | Serum 25 (OH)D level (ng/ml) |
|---|---|
| Severe Deficiency | <=5 |
| Deficiency | <=15 |
| Insufficiency | 15-20 |
| Sufficiency | 20-100 |
| Excess | >100 |
| Intoxication | >150 |
References
[edit | edit source]- ↑ Walter F., PhD. Boron (2003). "The Parathyroid Glands and Vitamin F". Medical Physiology: A Cellular And Molecular Approaoch. Elsevier/Saunders. p. 1094. ISBN 978-1-4160-2328-9.
- ↑ Adams JS, Hewison M (2010). "Update in Vitamin D". Journal of Clinical Endocrinology & Metabolism 95 (2): 471–8. doi:10.1210/jc.2009-1773. PMC 2840860. PMID 20133466.
- ↑ a b Invalid
<ref>tag; no text was provided for refs namedRiver - ↑ Bouillon R, Van Cromphaut S, Carmeliet G (2003). "Intestinal calcium absorption: Molecular vitamin D mediated mechanisms". Journal of Cellular Biochemistry 88 (2): 332–9. doi:10.1002/jcb.10360. PMID 12520535.
- ↑ Holick MF (2004). "Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease". The American Journal of Clinical Nutrition 80 (6 Suppl): 1678S–88S. PMID 15585788.
- ↑ Puchacz E, Stumpf WE, Stachowiak EK, Stachowiak MK (February 1996). "Vitamin D increases expression of the tyrosine hydroxylase gene in adrenal medullary cells". Molecular Brain Research 36 (1): 193–6. doi:10.1016/0169-328X(95)00314-I. PMID 9011759.
- ↑ Vitamin D The Physicians Desk Reference. 2006 Thompson Healthcare.
- ↑ Sarkar FH, Li Y, Wang Z, Kong D (2010). "The role of nutraceuticals in the regulation of Wnt and Hedgehog signaling in cancer". Cancer Metastasis Reviews 29 (3): 383–64. doi:10.1007/s10555-010-9233-4. PMC 2974632. PMID 20711635.
- ↑ "Hedgehog signaling and Vitamin D". Medscape.com. 2009-12-18. Retrieved 2010-03-25.
- ↑ Bell TD, Demay MB, Burnett-Bowie SAM (April 2010). "The biology and pathology of vitamin D control in bone". Journal of Cellular Biochemistry 111 (1): 7–13. doi:10.1002/jcb.22661. PMID 20506379.
- ↑ American Academy of Periodontology 2010 In-Service Exam, question A-27
- ↑ Standing Committee on the Scientific Evaluation of Dietary Reference Intakes Institute of Medicine. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington, DC: National Academy; 1997. 45. Gartner LM, Greer FR. Prevention of rickets and vitamin D deficiency: new guidelines for vitamin D intake. Pediatrics. 2003;111:908-10.
- ↑ Ross AC, Taylor CL, Yaktine AL, Del Valle HB. Dietary Reference Intakes for Calcium and Vitamin D. Committee to Review Dietary reference Intakes for Vitamin D and calcium. Food and Nutrition Board, Institute of Medicine 2010. The National Academies Press, Washington D.C.
- ↑ Rathi, N., & Rathi, A. (2011). Vitamin d and child health in the 21 st century. In N. Rathi (Ed.), From Rathi Children’s Hospital and Maternity Home, Akola; and *Seth GS Medical College and KEM Hospital, Parel; Mumbai 400 012; MS, India. (August ed., Vol. 48, p. 622). India: Indian Paediatrics.
• http://www.spine-health.com/conditions/osteoporosis/calcium-and-vitamin-d-requirements
Vitamin D can be obtained two ways either from sun exposure, as discussed before or from foods. Vitamin D starts out inactive as 25-hyrdoxyvitamin D, it is then hydroxylated through two processes to make it into a usable form for the body. The first hydroxylation occurs in the liver where vitamin D is converted to calcidiol. The second process of hydroxylation occurs primarily in the kidney and it activates it into the hormone we use known as calcitriol. The best way to figure out how much vitamin D is necessary for the body is by looking at the serum concentration. According to the Vitamin D Health Fact Sheet, a serum concentration of 25(OH)D is the best indicator of vitamin D status(National Institutes of Health). This serum concentration represents the status of vitamin D in our body, the amount of vitamin D that we absorb from the sun and foods. It is tested through our blood and it helps us know if we have enough vitamin d in our body to carry out certain functions such as metabolic functions. The serum concentrations of 25(OH)D are reported in nanomoles per liter (nmol/L). According to the table of: Serum 25-Hydroxyvitamin D [25(OH)D] Concentrations and Health, any levels over 30 nmol/l but less than 12 nmol/l lead to rickets in young children and osteomalacia in adults. The adequate levels of serum for bone and overall health in healthy individuals is between 20 -50 nmol/l (National Institutes of Health). Relating back to the Paleolithic era, this is when the naked ape hypothesis came to be. It demonstrated that the requirement for a certain 25(OH)D concentration circulating in our body was fixed into our genes during a time when we were constantly exposed to the sun.. This genome was optimized through Darwin’s theory of natural selection. The levels of 25(OH)D occurred in UV-rich conditions that can now be seen in people that spend most of their time outdoors under the hot sun. It seems to be that the concentration of the serum 25(OH)D was affected by the evolution of us losing fur and gaining clothing and changing from nomadic to sedentary lifestyles.
7.3.4 Deficiency
[edit | edit source]Vitamin D deficiency can be caused by not eating enough food high in vitamin d or not enough sunlight exposure. When this happens the chances of getting rickets gets increased. Rickets is a disorder where the bones become soft and weak and then begin to bow. The sorts of people who suffer most with vitamin d deficiency would be: • Those who live in areas with very little sunlight • Work in doors during the day • Are a vegetarian • Lactose intolerant • Do not have milk products in their diet
Rickets and osteomalacia are classic vitamin D deficiency diseases. In children, vitamin D deficiency causes rickets, which results in skeletal deformities. In adults, vitamin D deficiency can lead to osteomalacia, which results in muscular weakness in addition to weak bones. Populations who may be at a high risk for vitamin D deficiencies include the elderly, obese individuals, exclusively breastfed infants, and those who have limited sun exposure. Also, individuals who have fat malabsorption syndromes (e.g., cystic fibrosis) or inflammatory bowel disease (e.g., Crohn's disease) are at risk.
Vitamin D deficiency is more common among African Americans and Latinos; (the pigment melanin reduces the skin’s ability to make vitamin D in response to sunlight exposure. Some studies show that older adults with darker skin are at high risk of vitamin D deficiency). Other cases are when the kidneys cannot convert vitamin D to its active form as people age, their kidney are less able to convert vitamin D to its active form, thus increasing their risk to vitamin D deficiency.
Vitamin D is a fat soluble vitamin and its synthesis in the body is dependent on multiple factors like latitude, atmospheric pollution, clothing, skin pigmentation and duration and time of exposure to sunlight. The FAO/WHO Expert Consultation5 states that in most locations of the world between 42° N and 42°S latitude there is abundant sunshine. This is responsible for physiological production of Vit D endogenously in the skin from 7-dehydrocholesterol present in the subcutaneous fat. Thirty minutes of exposure of the skin over the arms and face to sunlight, without application of sunscreen, preferably between 10 am to 2 pm (as maximum ultraviolet B rays are transmitted during this time) daily is adequate to avoid Vitamin D deficiency.[1]
In order to treat the vitamin d deficiency you need to replace it by including it in your diet and by exposing yourself to the sunlight or supplements can be given. If this problem isn't sorted out promptly then the chances of rickets, bone pain, deformities and impaired growth are greater.
Other recommendations from the Institute of Medicine for vitamin D supplementation suggest 200 IU of vitamin D daily from birth through age 50 years, 400 IU/d for individuals age 51 to 70 years, and 600 IU/d for those age 70 years or older. These recommendations presume some sun exposure and vitamin D intake from food and are not adequate to treat vitamin D deficiency.
7.2.5 Toxicity
[edit | edit source]Toxicity
Vitamin D toxicity, also known as hypervitaminosis D, occurs when you have too much vitamin D in your system. Vitamin D is present in foods and is commonly synthesized in the skin using sunlight. However, vitamin D toxicity is usually the result of taking high doses of vitamin D supplements. This is largely due to the fact that the body is able to regulate the levels of vitamin D produced from sunlight and vitamin D is only naturally present in very few foods.[25]
Beginning symptoms include vomiting, nausea, and weight loss. Excess Vitamin D can later result in calcification. Calcification is the buildup of calcium in the blood which can lead to high levels of calcium in the tissue, bone and vascular system. Calcification can also cause high blood pressure and kidney damage as the kidney attempts to excrete excess calcium through urination.[26] Diagnosis for toxicity includes measuring serum Ca levels weekly, then monthly in the later process. Once diagnosis has been determined, vitamin D intake will be stopped and the patient will be treated with IV normal saline hydration. Bone resorption inhibitors such as corticosteroids or bisphosphonates will also be used to reduce calcium levels in the blood.[27]
when some one has consumed too much vitamin d it can cause very high calcium in the blood which in turn can cause kidney damage. There are a number of signs and symptoms that go with this which are: • Constipation • Decreased appetite • Vomiting • Dehydration • Fatigue
There are tests which can confirm the diagnosis such as blood tests and X-rays.
Assessment of Vitamin D
In the past measurement of serum vitamin D was limited by methodological differences (issues)17-19. With the evolution of 125I radioimmunoassay (RIA) for estimation serum 25-hydroxyvitamin D [25(OH)D] the methodological differences have vanished (disappeared) permitting an inter-laboratory comparison of the values. [The currently available assays have antibodies cospecific to both 25(OH) D2 and 25(OH)D3 and hence the terminology 25(OH)D assays are used. The laboratory normally estimates 25(OH)D levels and not 25(OH)D2 or 25(OH)D3].18-24 These advancements are limited by improper definition of vitamin D deficiency and hypovitaminosis D.[2]
Assessment of serum 25(OH)D requires a blood test, a procedure not routinely ordered by healthcare providers. Vitamin D status is declining (Looker et al.,2008), so it is important that testing be implemented when appropriate. A noninvasive screening tool could help determine the need for serum 25(OH)D testing,but currently, no validated, reliable, multi-item vitamin D screening tool exists that is intended for self-administration in community health/wellness settings.[3]
The only way to treat it is to stop taking in so much vitamin D and go and visit your GP as they can advise any further steps in treatment.
References
[edit | edit source]- ↑ Londhey, V. (2011). Vitamin d deficiency: Indian scenario. In V. JAPI (Ed.), (Vol. 59, p. 695). India: JAPI. doi:www.japi.org
- ↑ Harinarayanan, C., & Shashank, R. J. (2009). Vitamin d status in india – its implications and remedial measures. In C. JAPI (Ed.), JAPI-review article (Vol. 57, pp. 41). India: JAPI. doi:www.japi.org
- ↑ Looker, A. C., Pfeiffer, M., Lacher, D. A., Schleicher, R. L., Picciano, M. F., & Yetley, E. A. (2008). Serum 25-hydroxyvitamin D status of the US population: 1988–1994 compared with 2000-2004. American Journal of Clinical Nutrition, 88, 1519–1527.
1. Harinarayanan, C., & Shashank, R. J. (2009). Vitamin d status in india – its implications and remedial measures. In C. JAPI (Ed.), JAPI-review article (Vol. 57, pp. 40–49). India: JAPI. doi:www.japi.org
2. Londhey, V. (2011). Vitamin d deficiency: Indian scenario. In V. JAPI (Ed.), (Vol. 59, p. 695). India: JAPI. doi:www.japi.org
3.Standing Committee on the Scientific Evaluation of Dietary Reference Intakes Institute of Medicine. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington, DC: National Academy; 1997.
4. Gartner LM, Greer FR. Prevention of rickets and vitamin D deficiency: new guidelines for vitamin D intake. Pediatrics. 2003;111:908-10.
5. Ross AC, Taylor CL, Yaktine AL, Del Valle HB. Dietary Reference Intakes for Calcium and Vitamin D. Committee to Review Dietary reference Intakes for Vitamin D and calcium. Food and Nutrition Board, Institute of Medicine. 2010. The National Academies Press, Washington D.C
6. Rathi, N., & Rathi, A. (2011). Vitamin d and child health in the 21 st century. In N. Rathi (Ed.), From Rathi Children’s Hospital and Maternity Home, Akola; and *Seth GS Medical College and KEM Hospital, Parel; Mumbai 400 012; MS, India. (August ed., Vol. 48, p. 622). India: Indian Paediatrics.
7. Looker, A. C., Pfeiffer, M., Lacher, D. A., Schleicher, R. L., Picciano, M. F., & Yetley, E. A. (2008). Serum 25-hydroxyvitamin D status of the US population: 1988–1994 compared with 2000-2004. American Journal of Clinical Nutrition, 88, 1519–1527.
8. Dorland's Illustrated Medical Dictionary, under Vitamin (Table of Vitamins)
9. History of Vitamin D University of California, Riverside, Vitamin D Workshop.
10. Crissey SD, Ange KD, Jacobsen KL, Slifka KA, Bowen PE, Stacewicz-Sapuntzakis M, Langman CB, Sadler W, Kahn S (2003). "Serum concentrations of lipids, vitamin D metabolites, retinol, retinyl esters, tocopherols and selected carotenoids in twelve captive wild felid species at four zoos". The Journal of nutrition 133 (1): 160–6. PMID 12514284.
11. Hume EM, Lucas NS, Smith HH (1927). "On the Absorption of vitamin D from the Skin". Biochemical Journal 21 (2): 362–367. PMC 1251921. PMID 16743844.
12.C. Claiborne Ray (2005-05-17). "Sunshine Vitamin D". The New York Times. Retrieved 2013-03-08.
13. Holick MF (March 1995). "Environmental factors that influence the cutaneous production of vitamin D" (PDF). The American Journal of Clinical Nutrition 61 (3 Suppl): 638S–645S. PMID 7879731.
14. Yahav S, Buffenstein R (1993). "Cholecalciferol supplementation alters gut function and improves digestibility in an underground inhabitant, the naked mole rat (Heterocephalus glaber), when fed on a carrot diet". The British journal of nutrition 69 (1): 233–41. doi:10.1079/BJN19930025. PMID 8384476.
15. Stout SD, Agarwal SC (2003). Bone loss and osteoporosis: an anthropological perspective. New York: Kluwer Academic/Plenum Publishers. ISBN 0-306-47767-X.
16. Adams JS, Hewison M (2010). "Update in Vitamin D". Journal of Clinical Endocrinology & Metabolism 95 (2): 471–8. doi:10.1210/jc.2009-1773. PMC 2840860. PMID 20133466.
17. Bouillon R, Van Cromphaut S, Carmeliet G (2003). "Intestinal calcium absorption: Molecular vitamin D mediated mechanisms". Journal of Cellular Biochemistry 88 (2): 332–9. doi:10.1002/jcb.10360. PMID 12520535.
18. Holick MF (2004). "Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease". The American Journal of Clinical Nutrition 80 (6 Suppl): 1678S–88S. PMID 15585788.
19. Puchacz E, Stumpf WE, Stachowiak EK, Stachowiak MK (February 1996). "Vitamin D increases expression of the tyrosine hydroxylase gene in adrenal medullary cells". Molecular Brain Research 36 (1): 193–6. doi:10.1016/0169-328X(95)00314-I. PMID 9011759.
20. Vitamin D[dead link] The Physicians Desk Reference. 2006 Thompson Healthcare.
21. Sarkar FH, Li Y, Wang Z, Kong D (2010). "The role of nutraceuticals in the regulation of Wnt and Hedgehog signaling in cancer". Cancer Metastasis Reviews 29 (3): 383–64. doi:10.1007/s10555-010-9233-4. PMC 2974632. PMID 20711635.
22."Hedgehog signaling and Vitamin D". Medscape.com. 2009-12-18. Retrieved 2010-03-25
23. Bell TD, Demay MB, Burnett-Bowie SAM (April 2010). "The biology and pathology of vitamin D control in bone". Journal of Cellular Biochemistry 111 (1): 7–13. doi:10.1002/jcb.22661. PMID 20506379.
24. American Academy of Periodontology 2010 In-Service Exam, question A-27
25. Zeratsky, K. (2015). Vitamin D toxicity: What is vitamin D toxicity, and should I worry about it since I take supplements?. Mayo Foundation: Healthy Lifestyle.
26. Ross, C., Taylor, L., & Yaktine, L. (2011). Dietary Reference Intakes for Calcium and Vitamin D. National Center for Biotechnology Information, 6.
27. Johnson, L. (2014). Vitamin D: Vitamin D Toxicity. Merick Manual Professional Version.
External links
[edit | edit source]- http://www.telegraph.co.uk/health/healthnews/8443773/The-best-natural-sources-of-Vitamin-D.html
- http://www.nhs.uk/Conditions/vitamins-minerals/Pages/Vitamin-D.aspx
- http://www.mayoclinic.com/health/vitamin-d/NS_patient-vitamind
- http://www.sfgate.com/health/article/Vitamin-D-deficiency-and-how-to-avoid-it-4196666.php
- http://jop.ascopubs.org/content/6/2/97.full
- http://www.bocsci.com/vitamin-d5-cas-71761-06-3-item-453668.html
