Psychiatric Disorders/Printable version
| This is the print version of Psychiatric Disorders You won't see this message or any elements not part of the book's content when you print or preview this page. |
The current, editable version of this book is available in Wikibooks, the open-content textbooks collection, at
https://en.wikibooks.org/wiki/Psychiatric_Disorders
Introduction
What is Psychiatry?
[edit | edit source]Psychiatry is a branch of medicine that is concerned with the diagnosis and treatment of mental, emotional, and behavioral disorders.
However, it should also be noted that recent advances in the field have expanded its scope as the distinction between “psychiatric” disease and “medical” disorders has begun to blur. It is now widely recognized that psychiatric disease is an independent risk factor in the etiology of many disease states and disorders that have traditionally been the viewed as “medical” disorders. For example, depression is now known to increase the risk for cardiovascular disease. Furthermore, pharmacologic treatment of psychiatric disorders also plays a role in the iatrogenic etiology of medical disease. (for example, Diabetes Mellitus, cardiac arrhythmias, and Hypertension).
Development Status
[edit | edit source]This volume on Psychiatry is currently in the initial stages of development. Further development will be a project of the Educational Taskforce of the World Psychiatric Association.
For further information, please contact Dan Stein (dan.stein@uct.ac.za).
Timeline in Psychiatry
1550 BC
[edit | edit source]
The Ebers papyrus, one of the most important medical papyri of ancient Egypt, briefly mentioned clinical depression.
4th century BC
[edit | edit source]Hippocrates theorized that physiological abnormalities may be the root of mental disorders.
280 BC
[edit | edit source]Greek physician and philosopher Herophilus studies the nervous system and distinguishes between sensory nerves and motor nerves.
250 BC
[edit | edit source]
Greek anatomist Erasistratus studies the brain and distinguishes between the cerebrum and cerebellum.
705
[edit | edit source]The first psychiatric hospital was built in Baghdad.
11th century
[edit | edit source]Persian physician Avicenna recognized 'physiological psychology' in the treatment of illnesses involving emotions, and developed a system for associating changes in the pulse rate with inner feelings.
13th century
[edit | edit source]Bethlem Royal Hospital in London, one of the famous old psychiatric hospitals, was set up.
1590
[edit | edit source]Scholastic philosopher Rudolph Goclenius used the term psychology. Though often regarded as the "origin" of the term, there is conclusive evidence that it was used at least six decades earlier by Marko Maruliæ.
1656
[edit | edit source]Louis XIV of France created a public system of hospitals for those suffering from mental disorders.
1672
[edit | edit source]In English physician Thomas Willis' anatomical treatise "De Anima Brutorum", Psychology was described in terms of Brain Function.
1758
[edit | edit source]English physician William Battie wrote the Treatise on Madness which called for treatments to be utilized in asylums.
1808
[edit | edit source]Dr. Johann Christian Reil, German physician, anatomist, physiologist and psychiatrist, coined the term 'Psychiatry'.
1816
[edit | edit source]French physician Dr. Rene Laennec invented the Stethoscope.
1821
[edit | edit source]The element of Lithium was first isolated from Lithium Oxide and described by William Thomas Brande, an English chemist.
1893
[edit | edit source]Dr. Emil Kraeplin defined "Dementia Praecox", currently Schizophrenia.
1895
[edit | edit source]German physicist Wilhelm Conrad Röntgen discovered medical use of X- rays in medical imaging and was conferred the first Nobel Prize in Physics in 1901.
1899
[edit | edit source]Dr. Sigmund Freud published 'The interpretation of dreams'.
1901
[edit | edit source]Alzheimer
[edit | edit source]Dr. Alois Alzheimer, German psychiatrist and neuropathologist, identified the first case of what later became known as Alzheimer's disease.
Blood Types
[edit | edit source]Austrian biologist and physician, Dr. Karl Landsteiner discovered the existence of different human blood types and in 1930, he won the Nobel Prize in Physiology or Medicine.
1905
[edit | edit source]French Psychologists Alfred Binet and Theodore Simon created the Binet-Simon scale to assess intellectual ability, marking the start for standardized psychological testing.
1906
[edit | edit source]Dr. Ivan Petrovich Pavlov, Russian physiologist, psychologist, and physician, published his first Conditioning studies.
1908
[edit | edit source]The word schizophrenia was coined by Dr. Paul Eugen Bleuler, Swiss psychiatrist.
1929
[edit | edit source]Dr. Hans Berger, German neuropsychiatrist, discovered human electroencephalography.
1934
[edit | edit source]Dr. Manfred Joshua Sakel, Polish neurophysiologist and psychiatrist, introduced insulin shock therapy; a precursor to ECT.
1936
[edit | edit source]Otto Loewi, Austrian-German-American pharmacologist, won the 1936 Nobel Prize in Medicine, which he shared with Sir Henry Dale, for his discovery of Acetylcholine, the first neurotransmitter to be described.
1938
[edit | edit source]Dr.Ugo Cerletti, Italian neurologist and Dr. Lucio Bini, Italian psychiatrist, discovered Electroconvulsive Therapy.
1948
[edit | edit source]Lithium carbonate's ability to stabilize mood highs and lows in bipolar disorder was demonstrated.
1949
[edit | edit source]Dr. Antonio Egaz Moniz, neurologist at the Lisbon Medical School won Nobel prize for his work on psychosurgery / lobotomy.
1952
[edit | edit source]Chlorpromazine
[edit | edit source]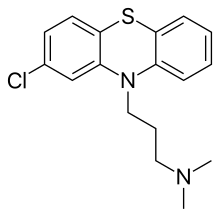
The first published clinical trial of Chlorpromazine was conducted at Ste. Anne Hôspital in Paris.
Manual
[edit | edit source]The APA published the first Diagnostic and Statistical Manual for Mental Disorders.
1960
[edit | edit source]The first benzodiazepine, Librium, was introduced, marking the rise of psychopharmacology.
1963
[edit | edit source]United States president John F. Kennedy introduced legislation delegating the National Institute of Mental Health to administer Community Mental Health Centers for those being discharged from state psychiatric hospitals.
1970
[edit | edit source]FDA approved Lithium for acute mania.
1972
[edit | edit source]Psychologist David Rosenhan published the Rosenhan experiment, a study challenging the validity of psychiatric diagnoses.
1977
[edit | edit source]The ICD-9 was published by the WHO.
1988
[edit | edit source]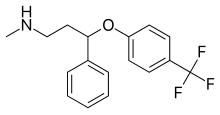
The first selective serotonin re-uptake inhibitor (SSRI) antidepressant, 'Prozac', was released and quickly became most prescribed.
1988
[edit | edit source]US President George Bush declared 1990s as "The decade of the brain".
2000
[edit | edit source]The No Free Lunch organization was founded by Dr. Bob Goodman, an internist from New York.
Basic Sciences Relevant to Psychiatry
Biochemistry - An amalgam of the scientific study of Biology (the science of living matter in all its forms) and Chemistry (the science concerned with the composition, properties, and reactions of substances) as they concern the processes (usually within the cells) which occur in living organisms.
Microbiology – The scientific study of a diverse group of simple life-forms including concerned with their structure, function, and classification. In medicine, more specifically, it is the study of disease-causing microorganisms that have been identified as a means to control their pathological effects.
Pharmacology – the study of the changes produced in living animals by chemical substances. In medicine this relates to the actions of drugs, (substances used to treat disease, i.e. medicines), and their effects on the human organism.
Genetics – the science of heredity, which is how the characteristics of living things are transmitted from one generation to the next. In medicine this relates to disease states resulting from chromosomal anomalies.
Neuroanatomy and physiology
to understand how it is that Brain is the substrate for Mind.
Psychology
to understand how behaviour, and internal states such as mood and thought, are regulated.
Sociology
to understand how individuals fit within society and are influenced by it.
Mental Health Status Examination
The purpose of this examination is to gather phenomenological data in an orderly way for purposes of diagnosis, checking of progress, note-taking, and communication.
It is largely based upon what a trained observer may see, and to a lesser extent upon what is described by the patient, although these must be combined. For instance, the comparison of affect, mood as reported by the patient, and countertransference phenomena is a key to the proper assessment of mood and psychotic disorders.
Notes about speech, language, and thought. In considering the mental state exam, speech may be confused with thought. The following definitions may assist:
Most correctly, speech is to be defined as the motor aspect of language. Speech would properly only be described according to articulation (how clearly each word is pronounced; slurring, running words together, etc.); anything else about utterances would be best categorized under Language or Thought.
Language is a system of symbols used to convey meaningful ideas. Language also includes how the ideas expressed fit in with the social situation: e.g. turn-taking. The neurology of language needs careful review by the student.
Thought and language are of course tightly linked concepts. Thought is the logical progression of ideas. Clearly the style of logic employed to link the ideas (the Form of thought) varies. Linkage may be only by sound, for instance: the so-called Klang association. e.g. "Mat, bat, cat."
The discussion below may be criticized as conflating speech with thought.
APPEARANCE
What does the patient look. like, smell like and sound like? Give a written description.
Self Neglect: cleanliness, shaven, make up, state of hair and clothes
Bizarre Appearance: secret documents openly displayed, special clothes or ornaments with symbolic significance, etc.
BEHAVIOUR
Involuntary movements: tics
Mannerisms
Stereotypes
Purposeful behaviour: pacing, fiddling
Congruity with the situation: does she act as if she understands the social conventions associated with the fact that she is being examined; e.g. when invited into the room, sits in what is obviously the examiner's chair.
RAPPORT
Includes Demeanour: threatening, seductive, friendly
AFFECT
Mood: inner emotional experience: can be inferred, but is best described
Affect: outer expression of mood
Level: elevated, lowered, euthymic
Range: restricted, increased, normal
Congruity: does the affect match what is being discussed?
Communicability: how readily does the observed affect and described mood cause a corresponding and similar feeling in the examiner? For instance, the moods of mania and depression are readily communicated. See Countertransference.
SPEECH
Slow Speech: Long pauses before answering, long pauses between words
Pressure of Speech: An increase in the amount of spontaneous speech as compared with what is considered ordinary or socially customary. The patient talks rapidly and is difficult to interrupt. Some sentences may be left uncompleted because of eagerness to get on to a new idea. Simple questions that could be answered at great length, so that the answer takes minutes rather than seconds and indeed may not stop at all if the speaker is not interrupted. Even when interrupted, the speaker often continues to talk. Speech tends to be loud and emphatic. Sometimes speakers with severe pressure will talk without any social stimulation and talk even though no one is listening. When patients are receiving phenothiazines or lithium carbonate, their speech is slowed down by medication, and then it can be judged only on the basis of amount, volume and social appropriateness. This disorder may be accompanied by derailment, tangentiality, or incoherence, but it is distinct from them.
Non Social Speech: Talks, mutters, whispers to self, out of context of conversation with examiner.
Muteness: Almost mute, (fewer than 20 words in all) Totally mute
Poverty of Speech (Poverty of Thought, Laconic Speech): Restriction in the amount of spontaneous speech, so that replies to questions tend to be brief, concrete, and unelaborated. Unprompted additional information is rarely provided. Replies may be monosyllabic, and some questions may be left unanswered altogether.
When confronted with this speech pattern, the interviewer may find himself frequently prompting the patient to encourage elaboration of replies. To elicit this finding, the examiner must allow the patient adequate time to answer and to elaborate his answer.
Example Interviewer "Do you think there is a lot of corruption in government?" Patient "Yeah seem to be" Interviewer "Do you think Haldeman and Ehrlichman and Mitchell have been fairly treated?" Patient "I don't know". Interviewer "Were you working at all before you came to the hospital?" Patient "No". Interviewer "What kind of jobs have you had in the past?" Patient "Oh some janitor jobs painting" Interviewer "What kind of work do you do?" Patient "I don't, don't like any kind of work.
That's silly". Interviewer "How far did you go in school?" Patient "I'm still in 11th grade". Interviewer "How old are you?" Patient "Eighteen”.
Neologisms: New word formation. A neologism is defined here as a completely new word or phrase whose derivation cannot be understood. Sometimes the term "neologism" has also been used to mean a word that has been incorrectly built up but with origins that are understandable as due to a misuse of the accepted methods of word formation. For purposes of clarity, these should be referred to as word approximations (discussed in the following section). Neologisms are quite uncommon.
Examples "I got so angry I picked up a dish and threw it at the geshinker". "So I sort of bawked the whole thing up".
Word Approximations (Paraphasia, Metonyms): Old words that are used in a new and unconventional way, or new words that are developed by conventional rules of work formation. Often the meaning will be evident even though the usage seems peculiar or bizarre (i.e.: gloves referred to as "handshoes", a ballpoint pen referred to as "paper skate" etc.). Sometimes the word approximations may be based on the use of stock words, so that the patient uses one or several words repeatedly in ways that give them a new meaning (i.e.: a watch may be called a "time vessel" the stomach a "food vessel" a television set a "news vessel" etc.). "One is called 'per God' and the other is called 'per the Devil"' miracle willed through God's 'turn horn' .... "Well, there is. a frequenting of clairvoyance ..." "Per God". "Per the Devil" and "turn horn" are neologisms; "frequenting of clairvoyance" is an example of ordinary words used idiosyncratically. Write down examples.
Disorder of Content of Speech: Three types of disordered content are specified: incoherence, flight of ideas and poverty. There are overlapping concepts and in each case, the effect is to make it very difficult to grasp what the patient means. However, the symptoms are defined in terms of specific components so that it should, in most cases, be possible to say whether one, two or all three symptoms are present. If in doubt, rate hierarchically; i.e., rate incoherence in preference to flight of ideas, and flight of ideas in preference to poverty of speech.
Incoherence of Speech: see Incoherence in section on Thought Form
Clanging: A pattern of speech in which sounds rather than meaningful relationships appear to govern word choice, so that the intelligibility of the speech is impaired and redundant words are introduced. In addition to rhyming relationships, this pattern of speech may also include punning associations, so that a word similar in sound brings in a new thought. Example "I'm not trying to make noise. I'm trying to make sense. If you can make sense out of nonsense, well, have fun. I'm trying to make sense out of sense. I'm not making sense (cents) anymore. I have to make dollars".
Poverty of Content of Speech (Poverty of Thought, Empty Speech, Alogia, Verbigeration, Negative Formal thought Disorder): Although replies are long enough so that speech is adequate in amount, it conveys little information. Language tends to be vague, often over abstract or over concrete, repetitive and stereotyped. The interviewer may recognise this finding_ by observing that the patient has spoken at some length but has not given adequate information to answer the question. Alternatively, the patient may provide enough information to answer the question, but require many words to do so, so that a lengthy reply can be summarised in a sentence or two.
Sometimes the interviewer may characterise the speech as "empty philosophising".
Exclusions This finding differs from circumstantially in that the circumstantial patient tends to provide a wealth of detail.
Example Interviewer "Tell me what you are like, what kind of person you are". Patient "Ah one hell of an odd thing to say perhaps in these particular circumstances, I happen to be quite pleased with who I am or how I am and many of the problems that I have and have been working on I have are difficult for me to handle or to work on because I am not aware of them as problems which upset me personally. I have to get my feelers way out to see how it is and where that what I may be or seem to be is distressing, too painful or uncomfortable to people who make a difference to me emotionally and personally or possibly on an economic or professional level. And I am I think becoming more aware that perhaps on an analogy the matter of some who understand or enjoy loud rages of anger, the same thing can be true for other people, and I have to kind of try to learn to see when that's true and what I can do about it".
Misleading Answers: Patient's answers are misleading because answers Yes or No to everything, or frequent self contradictions, or appears to be deliberately misleading. Do not include incoherence, flight of ideas or poverty of speech here.
Distractible Speech: During the course of a discussion or interview, the patient repeatedly stops talking in the middle of a sentence or idea and changes the subject in response to a nearby stimulus, such as an object on a desk, the interviewer's clothing or appearance, etc.
Example "Then I left San Francisco and moved to Where did you get that
tie? It looks like it's left over from the '50s. I like the warm weather in San Diego. Is that a conch shell on your desk? Have you ever gone scuba diving".
Stilted Speech: Speech that has an excessively stilted or formal quality. It may seem rather quaint or outdated, or may appear pompous, distant, or overpolite. The stilted quality is usually achieved through use of particular word choices (multisyllabic when monosyllabic alternatives are available and equally appropriate), extremely polite phraseology. ("Excuse me, madam, may I request a conference in your office at your convenience?"), or stiff and formal syntax ("Whereas the attorney comported himself indecorously, the physician behaved as is customary for a born gentleman").
Paraphasia, Phonemic: Recognisable mispronunciation of a word because sounds or syllables have slipped out of sequence. Severe forms occur in aphasia, milder forms may occur as "slips of the tongue" in everyday speech. The speaker often recognised his error and may attempt to correct it.
Example "I slipped on the lice and broke my arm while running to catch the bus"
Paraphasia, Semantic: Substitution of an inappropriate word during his effort to say something specific. The speaker may or may not recognise his error and attempt to correct it. It typically occurs in both Broca's and Wernicke's aphasia. It may be difficult to distinguish from incoherence, since incoherence may also be due to semantic substitutions that distort or obscure meaning.
INSIGHT
Does the patient know there is a problem; how does she assess her impairment, disability, and handicap due to the problem
how important is it to her;
does she want treatment;
how rational is her understanding of the problem and its treatment
COGNITIVE EXAMINATION
ORIENTATION
SPECIFIC TESTS
PHYSICAL EXAMINATION Special attention to:
the signs and causes of delirium
stigmata of drug use (acute: intoxication, and chronic, e.g. needle track marks, stigmata of alcohol and tobacco use) and abuse
stigmata of self harm, e.g. scars
general body habitus: obesity, degree of fitness
Neurological examination
COUNTERTRANSFERENCE
A term borrowed from psychoanalytic theory and practice, now used fairly generally to denote the therapist's own reactions to the interview. It is an essential part of the armamentarium of the therapist in all diagnostic and therapeutic encounters. Its components have been debated but may reasonably be said to include:
a) reactions arising from the therapist (such as empathy, sympathy, and thoughts, feelings, impulses etc. arising in the context of any state of mental health), and
b) mental states arising within, and communicated directly and literally from the patient. These may be experienced by the attuned therapist as unfamiliar, or not-self, although the distinction from one's own mental contents may be challenging even for experienced workers.
It will be apparent that the better a therapist knows him/herself, including his/her mental functioning and personality traits, the more valid a tool countertransference will be. Hence this tool, and one's general functioning as a psychiatrist, may be enhanced by a personal therapy.
Delirium, Dementia, and other Cognitive Disorders
Although most psychiatric disorders are presumed to have an underlying alteration in function, this group are separated off by having a suspected cause in another area of medical specialty. For example, delirium (wikipedia:Delirium), is commonly caused by alterations in brain oxygenation and would be better assessed by a physician to determine possible treatable causes. The organic disorders may have an underlying basis that is treatable or untreatable and treatment may or may not improve symptoms. This group includes Delirium, Dementia and other disorders listed below where they are proved to be secondary to a physical cause (e.g. a mood disorder secondary to changed thyroid function). Disorders which are caused by intoxication or withdrawal may also be consider ed under organic disorders, although we will consider substance use and misuse disorders separately
Dementia Definition: usually permanent disorder of memory, other cognitive functions and overall level of functioning. Major types of Dementia
Alzheimer's Disease Vascular Dementia Lewy Body Dementia
Psychotic Disorders
Psychotic disorders include the following disorders: Schizophrenia, Schizoaffective Disorder, Schizophreniform Disorder, Delusional Disorder, Brief Psychotic Disorder, and the Secondary Psychotic Disorders (Psychotic Disorder that are due to medical conditions or to substances). The central feature of these disorders is that they cause psychosis. Psychosis can be thought of as a loss of contact with reality. A person with a psychotic disorder is unable to evaluate properly what is or is not real.
In addition to the primary psychotic disorders, a number of other psychiatric disorders can cause a person to become psychotic. These include the mood disorders, such as psychotic depression, or mania with psychosis.
Thought Disorders
[edit | edit source]Psychotic disorders represent the failure of normal thought and, hence, they can be categorized as thought disorders. Thought disorders can be divided into different types. Most commonly, they are divided into disorders of process and disorders of content.
Disorders of Thought Process
[edit | edit source]Disorders of thought process involve a disturbance in the way one formulates thought. Thought disorders are inferred from speech, and often referred to as "disorganized speech." Historically, thought disorders have included associative loosening, illogical thinking, over inclusive thinking, and loss of the ability to engage in abstract thinking. Associative loosening includes circumstantial thought and tangential thought.
Other types of formal thought disorder include:
- Perseveration: the patient gets stuck on one idea or one thing and cannot move on from there
- Clanging: the connections between thoughts may be tenuous, and the patient uses rhyming and punning
- Neologisms: words that patients make up; often a condensation of several words that are unintelligible to another person
- Echolalia: the patient repeats back the words of other people, “parrots” people’s speech
- Thought blocking: stopping mid-thought and being unable to continue with the thought
- Word salad: an incomprehensible mixing of meaningless words and phrases.
- For a larger list of thought disorders, see this article
Disorders of Thought Content
[edit | edit source]Disorders of thought content include hallucinations and delusions.
Hallucinations are perceptions without external stimuli. They are most commonly auditory, but may be any type. Auditory hallucinations are often voices, mumbled or distinct. Visual hallucinations can be simple or complex, in or outside the field of vision (ex. "in head") and are usually of normal color rather than black and white. Olfactory and gustatory hallucinations generally occur together as unpleasant tastes and smells. Tactile or haptic hallucinations may include any sensation—for example, an electrical sensation or the feeling of bugs on skin (formication).
Delusions are fixed, false beliefs, not amendable by logic or experience. There are a variety of types. Delusions are most commonly persecutory, but may be somatic, grandiose, religious or nihilistic. No one type of delusion is specific to any particular disorder (such as schizophrenia). Hallucinations and delusions are common across all cultures and backgrounds; however, culture may influence their content. Culture and religion must be considered when evaluating whether an event is a delusion or hallucination. In this context, a good rule of thumb is that if other people endorse it, it may not be a delusion or hallucination.
Mood Disorders
The mood disorders are any disorder that can cause an increased or decreased mood. Most of the major mood disorders are characterized by the presence of one or more syndromes: a depressive episode, a manic episode, a hypomanic episode or a mixed episode.
One can picture the possible range of moods on a continuum from dysphoria on one pole to euphoria on the other. Euthymia or a “normal mood” would be in the middle.
Unipolar Disorders
[edit | edit source]Disorders that affect only one pole are sometimes called “unipolar disorders.” In theory these could affect either pole, however, in practice this term generally refers to depressive disorders.
The unipolar mood disorders include Major Depressive Disorder, Dysthmia, and the Secondary Depressions.
Bipolar Disorders
[edit | edit source]Bipolar Disorders can cause both euphoria and dysphoria. Disorders in this category include Bipolar Disorder, Cyclothymia, and the Secondary Manias.
Anxiety Disorders
The anxiety disorders include disorders with symptoms of anxiety or excessive worrying, phobias and panic attack. Specific disorders include Panic Disorder, Agoraphobia without History of Panic Disorder, Specific Phobia, Social Phobia, Obsessive-Compulsive Disorder, Posttraumatic Stress Disorder, Acute Stress Disorder, Generalized Anxiety Disorder, and the Secondary Anxiety Disorders, Meaning, definition, cause, symptoms, preventions and treatments of Anxiety.
Anxiety is not, it itself, pathological, and in the right situation, appropriate anxiety is a necessary survival adaptation, motivating an individual to avoid potential or impending harm. One way to think of anxiety is as a warning signal, telling us of potential danger or harmful situations. Anxiety disorders are present when this warning system is not working properly: it may be overly sensitive, and cause the individual to overreact to minor or nonexistent dangers, or it may create so severe a reaction that the individual is too disabled to cope with the potential harm.
Anxiety involves various psychological and physical symptoms. The individual feels anxious and fearful. This is accompanied by various physical manifestations: restlessness, psychomotor agitation, shortness of breath, hyperventilation, stomach upset, chest pain and diaphoresis. Thought and cognition can be affected: a moderate amount of anxiety can actually be good for attention and concentration, however too much tends to make one distracted.
Anxiety disorders are the most prevalent of psychiatric disorders. Community samples, such as the Epidemiological Catchment Area Project, found surprisingly high lifetime prevalences (Figure 1). Clinical samples have shown anxiety disorders to be a very common reason for presentation to primary care doctors and emergency departments.
Anxiety disorders seem more common in women. They may decrease with age, and they can present differently at different ages. In children, an anxiety disorder can manifest as separation anxiety (“school phobia”). Elderly patients may tend towards somatic presentations (“stomach problems,” headaches, sleep problems).
Substance abuse disorders
Substance Abuse
Phenomenology
[edit | edit source]There are a number of syndromes and disorders associated with the general concept of substance abuse. Some of the most common are:
- Intoxication. A reversible, substance-specific physiological and behavioral changes due to recent exposure to a psychoactive substance.
- Addiction. A compulsion to use a drug, usually for its psychic, rather than therapeutic, effects.
- Tolerance. The decline in potency of a drug experienced with continued use, so that higher doses are needed to achieve the same effect. This is a receptor-mediated effect, typical of many psychoactive drugs.
- Physical Dependence. The development of withdrawal symptoms once a drug is stopped.
- Withdrawal. A physiological state that follows cessation or reduction in the amount of a drug used. Generally, these effects are the opposite of the drug’s normal effects.
- Substance Dependence. In the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), this is “a maladaptive pattern of substance use with adverse clinical consequences.”
- Substance Abuse. According to DSM-IV, this is “a maladaptive pattern of use that causes clinically significant impairment.” Symptoms of substance abuse have not met the criteria for substance dependence and do not include tolerance and withdrawal (which can, but do not have to be, features of substance dependence).
- Alcohol intoxication. This refers to the physiological and behavioral response to alcohol use that includes disinhibition, emotional lability, impaired coordination, slurred speech, ataxia, coma, and/or blackouts.
- Alcohol withdrawal. This is the physiological state that results following cessation of alcohol use; it may be uncomplicated (causing tremulousness, anxiety, and/or increased heart rate) or cause potentially serious complications such as seizures and/or delirium tremens (all of which are discussed further below).
- Alcoholism. Though not in DSM-IV (where the term “alcohol dependence” would be used) is remains commonly used by medical clinicians and substance abuse experts. It can be defined as a repetitive, but inconsistent and sometimes unpredictable loss of control of drinking which produces symptoms of serious dysfunction or disability.
Epidemiology
[edit | edit source]Use of psychoactive substances is common in society, and is often socially acceptable, or at least tolerated. Historically, psychoactive substances have served a variety of purposes, including medicinal, social, recreational and religious. In the US, 90% of people report some alcohol use, 80% report some caffeine use, 25% report use of tobacco products, and 37% report having used illicit substances (at least once in their lives). Dependence and Abuse are also very common (13.6% in ECA).
Alcohol
[edit | edit source]Over 10 million Americans are alcoholics; over 8 million are "problem drinkers." Only 3% of alcoholics are on skid row. Alcoholism is reportedly more common in rural areas and in the undereducated. It is more common in males than females, and more common in adults than teens/kids. However, teenage alcoholism studies show that 15% of high school students are reported to have 5 or more drinks per occasion at least once a week, and 31% of high school students were intoxicated 6 or more times in the past year.
Social/economic factors are considerable in that people in low socioeconomic status are less likely to drink, but more likely to misuse if they do. Drinking is associated with unstable work and family circumstances. Additionally, one should not forget the effect of substance abuse on families. Forty three percent of US adults report exposure to alcoholism in their families. Divorced or separated adults are 3 times as likely as married persons to report having been married to an alcoholic or problem drinker. Additionally, the cost to society is of great importance; alcohol-related deaths are the third leading cause of death in the US, after cancer and heart disease. There are 98,000 alcohol-related deaths per year. Furthermore, it is estimated that the medical complications and associated disability from alcohol abuse costs society $86 billion (along with $58 billion in costs from other substances). Alcoholism is also a major cause of other medical illnesses and injuries. Alcohol may be involved in 20-50% of hospital admissions, though these often go unrecognized. It contributes to 18-20% of ER visits, causes 80% of liver cirrhosis, and 33% of suicides are alcohol-related.
Cultural differences are also apparent in that alcoholism rates vary in different countries. Countries with high rates include Russia, France, Scandinavia, Ireland, and Korea. Those with low rates include China, Islamic countries, and Mediterranean countries
Other Substances
[edit | edit source]The lifetime prevalence of abuse for substances other than alcohol is as follows:
- Amphetamines: 2%
- Cannabis: 4%
- Cocaine 0.2% (1981 data, probably higher now)
- Hallucinogens: 0.3%
- Opioids: 0.7%
- Sedative hypnotics: 1.1%
Etiology
[edit | edit source]The reward pathway and addiction
[edit | edit source]There is considerable research interest in the notion of a common “reward pathway” in the human brain that may be responsible for the pleasurable feelings experienced by humans in response to both natural stimuli (i.e. food, water, sex) and artificial (i.e. drugs). The major structures of this postulated reward pathway include the ventral tegmental area (VTA), the nucleus accumbens, and the prefrontal cortex. The VTA consists of dopamine-containing neurons that project to both the nucleus accumbens and prefrontal cortex. Thus, it is believed that dopamine has a considerable role in addiction, and indeed, a number of illicit drugs cause increased release of dopamine at these synapses. The most recent research indicates that the reward pathway may be important in both obtaining a reward, and in the associated craving. Opioids, cocaine, and nicotine have been shown to potentiate dopamine release in the reward pathway, and alcohol has been shown activate this pathway indirectly through potentiation of neural activity in the globus pallidus (which in turn connects to components of the reward pathway).
Patterns of cigarette smoking provide an interesting perspective on addiction. It is believed that smokers work, consciously or unconsciously, to maintain blood nicotine levels within the “therapeutic window” by a process referred to as nicotine regulation. For example, the smoker can manipulate the dose of nicotine on a puff-by-puff basis (“finger tip control”). Evidence for this comes from studies of low tar, low nicotine cigarettes. Research has convincingly demonstrated that smokers will compensate for low nicotine yields by smoking more effectively—blocking filter holes to prevent ventilation of smoke; smoking more of the cigarette; inhaling more rapidly and deeply; and smoking a larger total number of cigarettes.
The route of delivery also has implications for addictive potential. For example, with cocaine use, smoking the drug causes an increased rate of its delivery to the brain compared to snorting; hence the greater addictive potential of freebase and crack in patients with cocaine dependence. For nicotine, compared to other forms of its administration, cigarettes offer the most efficient delivery and the fastest spike in blood nicotine levels. Likewise, the subjective effects of smoking a cigarette are greater than the subjective effects after nicotine exposure to the nicotine gum or transdermal patch (types of nicotine replacement therapy to be discussed later).
Alcoholism and genetics
[edit | edit source]While 51% of cases of alcoholism are non-familial, genetics has been well established in alcoholism, particularly among young male alcoholics. Any drinking carries with it a 5-10% risk of becoming alcoholic. For children of alcoholics, having one parent with alcoholism is associated with a 20% risk of alcoholism in the child. With two parents, the risk is 20-50%. Sons of father are at greater risk, at 50%. If the father is a severe alcoholic and criminal, there is a 90% risk in his son. Children of alcoholics are also at risk for other substance use disorders.
Adoption studies and twin studies have shown that alcoholism concordance among identical twins is twice that of fraternal. The Danish Adoption Study (1974), in which adopted sons of alcoholics were raised by non-alcoholic foster parents, showed that these children still had increased risk of alcoholism.
Sons of alcoholics show a number of physiological abnormalities, including abnormal EEG's associated with drinking compared with normal subjects and other abnormal brain wave studies (such as evoked potentials). In addition, there exist abnormal hormonal response patterns in sons of alcoholics.
Some genetic differences may relate to inherited variations in the rate of metabolism. For example, decreased gastric oxidation of alcohol in women causes a higher blood alcohol level (BAL) in woman than in men. There has also been report of an association with a mutation on the D2 dopamine receptor gene on chromosome 11. This likely acts not as "causer," but rather a modifier.
Pathology
[edit | edit source]Psychoactive effects relate to the direct effect of drug on receptors in the central nervous system. Thus, it is important to understand the pharmacokinetics of a drug: its routes of administration, absorption, metabolism, binding capacity, and excretion. Receptors have been identified for a number of substances—caffeine and cannabis, for example. Others substances act more nonspecifically—alcohol and inhalants, for example, act by dissolving into cell membranes, particularly in the central nervous system.
Pharmacodynamics: the following substances are listed with their receptors:
- Caffeine: adenosine
- Cannabis: THC receptor
- Hallucinogens: serotonin, NMDA
- Nicotine: nicotinic cholinergic receptors
- Opioids: opioid receptors
- Phencyclidine: NMDA
- Sedatives: chloride channel (GABA receptor)
Alcohol
[edit | edit source]Alcohol is generally thought to act by dissolving into cell membranes, specifically in the central nervous system. There is also some evidence that alcohol may potentiate the effects at neural synapses with GABAA receptors, similar to drugs such as benzodiazepines. Compared to benzodiazepines and other similar sedative drugs, however, alcohol use requires higher blood concentrations to achieve a comparable level of intoxication. Blood alcohol levels represent the concentration of alcohol in the blood and are typically measured in acutely intoxicated patients presenting for medical care (such as in emergency departments). The rate of increase in BAL is inversely related to the rate of gastric emptying; hence the reason for not drinking on an empty stomach. About 90% of patients with a BAL greater than 0.15% will show gross intoxication (with symptoms involving speech and gait), loss of consciousness can occur at 0.30%, and respiratory depression may be seen at about 0.45% (potentially resulting in death). Other acute effects of alcohol at the cellular level include ADH antagonism (the “happy hour diuresis”), potentiation of gastric acid secretion (increasing the risk for gastritis), increased peripheral vasodilation and flushing (a centrally-mediated effect), and increased levels of HDL, triglycerides, and uric acid.
Alcohol metabolism follows zero-order kinetics, meaning that a constant amount of the substance is metabolized per unit of time. The steps involved in hepatic alcohol metabolism are as follows:
Ethanol acetaldehyde acetate
The enzymes involved in this reaction are alcohol dehydrogenase (1st step) and acetaldehyde dehydrogenase (2nd step). As noted above, in women the rate of activity of alcohol dehydrogenase is lower, thus causing increased BAL levels. Alcohol metabolism can also be modified by hepatic microsomal enzymes that use NADPH. Acutely, alcohol use can inhibit hepatic p450 enzymes, thus transiently increasing the levels of concurrently taken drugs such as diazepam. With chronic use, however, alcohol can induce hepatic p450 enzymes, thus causing an increase in its own metabolism along with other drugs eliminated by this route. This may provide one cellular-based mechanism of tolerance that occurs with long-term users.
Cocaine
[edit | edit source]Cocaine acts in the brain by inhibiting catecholamine reuptake, thus increasing the availability of DA and NE in the synaptic cleft. As described above, the potentiation of DA activity in regions of the brain such as the nucleus accumbens may be responsible for cocaine’s addictive properties as well as its euphoriant effects. Dopaminergic activity is thought to also underlie the hallucinations (often tactile) sometimes seen during cocaine intoxication. Additionally, increased NE activity in the brain may cause symptoms of psychomotor agitation, including stereotypic or repetitive behaviors such as pacing, nail-biting, and scratching. This may be related to the binding of cocaine in areas such as the caudate nucleus. In addition, cocaine has peripheral effects on the body, augmenting sympathetic nervous system activity and causing tachycardia, pupillary dilation, and hypertension. Cocaine-mediated vasoconstriction can also produce angina, and in rarer instances, sudden cardiac death. Note that the effects of other substances on the body, particularly amphetamines, can mimic cocaine intoxication. Amphetamines enhance the release of NE and DA from the axon terminal, thus working similar to cocaine by increasing their availability in the synaptic cleft.
Nicotine
[edit | edit source]Receptors: Nicotine in tobacco exerts its actions on physiology and behavior by binding to nicotinic acetylcholine receptors (nAChRs), ion-gated channels that are normally responsive to endogenous acetylcholine. These receptors are found in the central nervous system and in the periphery (ANS, neuromuscular junction), and they are all involved in the physiological responses to tobacco. Each class of receptors generally contains different subunits, and experiments using gene knockout mice have indicated that certain subunits are specifically implicated in nicotine dependence. In time, this information may help to understand individual differences in response to nicotine and therefore nicotine dependence (e.g., those smokers with more or less of the specific nicotinic receptors), and it might help in tailoring new pharmacologic treatments which specifically target these receptors (e.g., by blocking or antagonizing their function, making nicotine less reinforcing).
It is also important to understand the dynamics of receptor function in relation to smoking and blood/brain nicotine levels. Neuroreceptors can become more sensitive for various reasons and they can also proliferate, both of which can be referred to as upregulation. Typically, one observes upregulation of receptors as a compensatory response to low levels of a neurotransmitter. Downregulation refers to the opposite, reduced sensitivity or fewer receptors, which in turn serves to compensate for excess levels of a neurotransmitter.
In the case of nicotinic receptors, the story is a little more complicated, and can be explained as follows: upon smoking a cigarette, a small pulse of nicotine activates nAChRs that directly or indirectly induce dopamine release, thus providing a pleasurable effect. With continued use, nicotine builds up to a slow steady-state concentration that causes significant nAChR desensitization and, over time, inactivation. There is evidence that nicotinic receptor turnover decreases following inactivation, leading to an increased number of nAChRs. In between cigarettes, during sleep, or under conditions of abstinence while attempting to stop smoking, nicotine levels drop and a portion of the inactive nAChRs recover to a responsive state. Because of the increased number of nAChRs that have now become responsive, some cholinergic systems become hyperexcitable to acetylcholine, contributing to the drive for the next cigarette. Thus, smokers may medicate themselves with nicotine to regulate the number of functional nAChRs. Note that this is still only a theoretical model, but it explains the powerful reinforcement experienced when smoking after a period of abstinence, even overnight. Understanding receptor function can also explain the rapid development of tolerance to nicotine’s effects, which would drive continued smoking.
Effects on the body: The effects of nicotine on the body are widespread. In the CNS, nicotine causes direct activation of ACh receptors, which when activated in regions such as the hippocampus can improve short-term memory and cognition/attention. Additionally, via activation of ACh receptors, nicotine can potentiate the release of dopamine (promoting its addictive properties, as described above), NE (promoting stimulation and arousal), and endogenous opioids (promoting stress-reducing and analgesic effects). There is also evidence that a component of tobacco (not nicotine) may inhibit the enzyme monoamine oxidase (MAO), which normally breaks down neurotransmitters such as dopamine, serotonin, and norepinephrine. Peripheral effects of nicotine are considerable and include increased heart rate, increased blood pressure, vasoconstriction, increased metabolic rate and lipolysis, skeletal muscle relaxation, and increased ACTH release and adrenal steroid production. Nicotine is rapidly cleared from the brain, and has a short half-life in the blood (with p450 liver metabolism to cotinine, the active metabolite), both which are factors that could partially account for the need for constant dosing.
Diagnosis
[edit | edit source]Classes of psychoactive substances recognized in DSM-IV include alcohol, amphetamines and related drugs, caffeine, cannabis, cocaine, hallucinogens, inhalants, nicotine, opioids, phencyclidine and related drugs, and sedatives. Polysubstance abuse occurs in which three or more categories of drug are abused (not including nicotine). Other drugs of abuse can include steroids, nitrates, and anticholinergics, to name a few. The criteria for diagnosis are as follows:
Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) Definitions
[edit | edit source]DSM-IV defined Substance Dependence is a maladaptive pattern of substance use. Criteria for diagnosis include three of following over a 1 year period:
- Tolerance
- Withdrawal
- Use in larger amounts than intended
- Persistent desire or unsuccessful attempts to cut down
- Time spent in activities necessary to get substance, taking substance or recovering from its effects.
- Social, occupational or recreational activities given up as a result of the substance
- Continued substance use despite knowledge of having a problem
Note that these patients don't need to have physical dependence. The definition of substance dependence is basically equivalent to "addiction," which is not used in DSM.
DSM-IV Substance Abuse is a maladaptive pattern of substance use leading to impairment. Criteria include one or more of following over 12 months:
- recurrent substance use resulting in a failure to fulfill role obligations (work, school, home)
- hazardous use (driving while intoxicated)
- related legal problems
- continued use despite persistent problems relating to the substance
It is important in the case of substance abuse to rule out substance dependence (which takes precedence).
DSM-IV Substance Intoxication is a reversible substance-specific syndrome due to recent exposure to a substance. Maladaptive behaviors or psychological changes can develop due to the substance and are not due to another medical/mental condition.
DSM-IV Substance Withdrawal is a substance-specific syndrome due to cessation or reduction in substance use that has been heavy and prolonged. Withdrawal causes distress/impairment, and is not due to another medical/mental condition.
Alcohol
[edit | edit source]Aside from classification according to DSM-IV criteria, other schemas of substance use/abuse exist as well. One such schema includes alcohol patterns. The so-called "alpha" pattern is one of continual excessive use when under stress, with no dependence and no loss of control. The "beta" pattern is one of heavy social drinking with physical complications, such as cirrhosis, but no dependence. The "delta" pattern is that of heavy daily drinking, but no loss of control. This is the more common type in Europe, for example in France. The "epsilon" pattern is defined as binge drinking, and the "gamma" pattern is that of physical dependence with loss of control. This is a more common type in the US.
Diagnostic tools for detecting alcoholism include administering the CAGE Questionnaire, and collecting other relevant historical data.
- The CAGE Questionnaire:
- Have you ever felt the need to Cut down on your drinking?
- Have you ever felt Annoyed by criticisms of your drinking?
- Have you ever had Guilty feelings about your drinking?
- Have you ever taken a morning Eye opener?
Some historical “red flags” might include (1) a pattern of unexplained job changes; (2) vague, defensive or evasive responses to alcohol-related questions; (3) DUI convictions; or (4) multiple unexplained traffic accidents. In addition, patients with alcoholism may have a history of impulsive behavior, fighting, or falls and scrapes, blackouts, binge drinking, or delirium tremens (DT’s). A history of drinking to relax or sleep is significant, as is a history of family chaos and instability. Relevant physical data to collect include the obvious stigmata of alcohol or drug use. For alcohol use, this may include spider angiomas, ruddy nose and face, peripheral neuropathies, liver disease, or cerebellar dysfunction. Additionally, patients may experience symptoms of gastric irritation related to acute or chronic alcohol use. For other drugs, this may be cutaneous abscesses and track marks (in IV drug abusers), or nasal lesions (cocaine).
Relevant laboratory data to collect for diagnostic purposes in alcoholism include a complete blood count and liver enzymes. Lab abnormalities may relate to malnutrition and organ damage, and may be expressed as leukopenia, macrocytic anemia, target cells (liver damage), thrombocytopenia, and bone marrow suppression. CAMP (cyclic adenosine monophosphate) levels in white blood cells of alcoholics are three times normal. Liver enzymes are abnormal in chronic alcoholism. Substance use can be easily detected via toxicology screens, in which urinary metabolites of several drugs are measured. It is important to observe directly the sample collection process. In addition, it is important to note the risk of false positives. One needs to confirm findings with a second test on the same sample using different analytic method (for example, poppy seed ingestion can cause false positive screens for opiates). Informed consent is crucial in toxicity screens.
Differential
[edit | edit source]"Normal use" is the main component in the differential of substance abuse. However, this brings up the question of what is normal. Perhaps the most important differential is between those patients who are addicted to drugs, and those who are merely physically dependent. The difference lies in the definition of addiction. For example, a patient with chronic pain, who is using regular opioids to alleviate pain, is probably physically dependent on the opioids, in the sense that the patient is probably tolerant to opioids, and would likely go into withdrawal if the opioids were suddenly stopped. However, such a patient does not necessarily show the compulsive behaviors associated with addiction. Furthermore, if the patient is taking the opioids for their analgesic, rather than euphoriant effects, then one cannot really say that the patient is addicted to antidepressants. Other differentials to consider in a patient with suspected substance abuse includes delirium along with other Axis I psychiatric conditions (which are often comorbid).
Comorbid Disorders And Complications
[edit | edit source]Medical Comorbidities
[edit | edit source]Alcohol
[edit | edit source]Withdrawal. Though generally uncomplicated, alcohol withdrawal can progress to delirium tremens (DTs), 10% of which are fatal. It is important to understand the differences between uncomplicated withdrawal and delirium tremens. Also, note that the hallucinations found in both of the above conditions are typically visual or tactile in nature, which may be distinguished from the auditory hallucinations of a distinct entity termed alcohol hallucinosis (described later).
Seizures. Seizures are common with high levels of alcohol use, independent of withdrawal.
Alcoholic Hallucinosis. Hallucinations can occur after drinking cessation in patients with alcohol dependence. These occur in a clear sensorium, and are not part of DTs. They are usually auditory hallucinations with persecutory content, and they can become chronic. Wernicke's encephalopathy: An acute neurological syndrome associated with long term alcohol abuse, the condition consists of delirium and the following triad of symptoms: ataxia, nystagmus and opthalmoplegia. It is thought to result from the thiamine deficiency that can result from chronic alcoholism. The treatment is, of course, to give thiamine (typically, it is given with folate).
Dementia. Dementia is common in patients with alcoholism. Most classic is the Korsakoff's Dementia (sometimes called Korsakoff's Psychosis, but that is a misnomer). This is characterized by an extremely poor short term memory--much worse than with Alzheimer's. Often associated with the memory losses are confabulations, though this is nonspecific to any dementia. More common is a more "run of the mill" type of dementia; usual called simply alcohol dementia, or dementia due to alcohol dependence. There remains some debate as to whether the dementia associated with alcoholism is due to a neurotoxic effect of alcohol itself, or to accessory problems (e.g., malnutrition, vitamin deficiencies).
The dementia associated with alcoholism is most likely irreversible. In the case of Korsakoff’s, the thiamine and folate are usually given, which do generally improve the Wernicke’s syndrome, but the memory disorder generally remains.
Fetal Alcohol Syndrome. FAS is due to heavy alcohol use during pregnancy. There is a high incidence in alcoholic mothers. Seventeen percent of births to alcoholic mothers are stillborn or die shortly after birth. Twenty percent have some defects, and 32% show fetal alcohol syndrome. Of those children with fetal alcohol syndrome, less than 6% are able to function normally in schools, and most never hold a job. (see is link for FAS
Withdrawal from other drugs
[edit | edit source]Unlike alcohol withdrawal, the course of withdrawal is generally not life-threatening in most of the other drugs of abuse described above. However, withdrawal in these instances may be very uncomfortable for the patient. Nicotine, for example, causes symptoms of irritability, headache, anxiety, increased heart rate, cravings, and (most concerning for many) weight gain. Women tend to gain more weight than men do during withdrawal. Most symptoms send to subside within two weeks on average, with considerable variability, but cravings and appetite increases may persist for much longer periods of time. Cocaine withdrawal also produces a number of symptoms, including hypersomnolence, fatigue, depression, intense cravings, and in some cases, suicidality. Note that the course of benzodiazepine withdrawal can mimic that of alcohol withdrawal (including seizures, DTs, or death), as both substances utilize biochemical mechanisms of action. Thus, benzodiazepine detoxification is approached with the same vigilance as in patients withdrawing from alcohol.
Psychiatric Comorbidities
[edit | edit source]ECA data suggested that 53% of those with a substance disorder had a comorbid mental disorder. Some of these mental disorders include antisocial personality disorder (11x higher than the general public), anxiety disorders (panic disorder, generalized anxiety disorder, and phobias), and depression. Most often, depression is secondary to alcoholism. It generally improves with abstinence, though some dysphoria may remain. Depression affects 13% of female alcoholics. Alcoholism is also more common in patients with schizophrenia and bipolar disorder. Attention Deficit Disorder may predispose to alcoholism, but this is a controversial topic.
Course
[edit | edit source]General principles dictate that alcoholism is often worse if familial. There are probably high incidences of (unreported) spontaneous remission. This complicates evaluation of different treatments. Drug abuse patterns are influenced by social and cultural factors and, compared with alcohol abuse, fluctuate over time.
Alcoholism typically has an exacerbating and remitting course, with periods of relative or complete abstinence. 2-3% of alcohol dependents become abstinent per year. Onset of alcoholism rarely begins after 45. Thirty percent of college problem drinkers are alcohol dependent 20 years later. The first hospitalization for alcohol tends to occur earlier in men (age 30 to 40). Abuse of cocaine and stimulants has a rapidly progressing course: from use to abuse and dependence. This is particularly true when the drugs are administered by the more potent routes (injection, inhaled). Oral and intranasal routes of ingestion show slower progression. Cannabis use rarely progresses to abuse and dependence if used alone. Hallucinogens very rarely progress to dependence. Opioid dependence represents a lifelong, chronic pattern. Abuse of sedative hypnotics can remit, either spontaneously or with treatment.
Personality disorders
The personality disorders are not disorders in the same sense as the other psychiatric disorders, and to reflect this, the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) lists them under a separate axis, Axis II. For this reason, they are sometimes referred to as “Axis II Disorders.” Rather than discrete disorders in the sense of major depression or schizophrenia, they are more patterns of maladaptive behaviors. They are disorders, however, in the sense that they do represent somewhat consistent clusters of symptoms, have a predictable course, and predictable responses to treatment. In addition, the disruptions they can cause in a person’s social and/or occupational functioning legitimizes their status as true disorders.
Working Definitions
[edit | edit source]- Personality Trait. A stable, recurring pattern of human behavior.
- Personality Type. A constellation of personality traits recognizable as a frequent and familiar combination – e.g. the compulsive personality, characterized by preoccupations with work, detail, order, time, money, and cleanliness.
- Personality Disorder. A constellation of personality traits, which are inflexible and maladaptive. These traits lead to difficulties in work or interpersonal relations, and can cause subjective distress.
- Neurosis. An unfashionable term for a non-psychotic mental disorder that causes the patient unpleasant feelings (including anxiety, depression, pathological shame or guilt). Many disorders formerly called neuroses are now incorporated into more major mood disorders, such as generalized anxiety disorder, dysthymia, adjustment disorder, obsessive-compulsive disorder, etc.
Speculations on Etiology
[edit | edit source]Personality is formed through an interaction of genetic and developmental influences. Severe personality disorders generally imply a mood disorder, mild neurological abnormality (such as attention deficit disorder or learning disability), or a family history of alcoholism or personality disorder, plus some kind of early loss, trauma, or abuse. If the developmental history is apparently benign, the likelihood of an affective or organic factor is even greater.
Personality traits that are maladaptive in adulthood may have been more adaptive in childhood. In some cases, it is possible to see how troublesome personality traits were reinforced by the family environment. However, it may happen that initially adaptive behaviors become counterproductive in adulthood, particularly if the environment has changed. Appreciation of the Role of Early Trauma in Severe Personality Disorders
Several studies show increased prevalence of childhood abuse, incest, or neglect, early loss, or family alcoholism in hospitalized patients with severe personality disorders.
Chronic post-traumatic stress disorder may produce symptoms that aggravate the personality disorder. Developmental histories of patients with severe personality disorder must attend to potential trauma, abuse, and neglect. Specific therapeutic attention to traumatic events may be crucial to success of treatment.
Diagnosis
[edit | edit source]Making a Personality Diagnosis
[edit | edit source]Making a diagnosis of a personality disorder can be difficult. It generally requires observing an individual over time, and the reliability of cross sectional diagnosis of a personality disorder is poor. Under sufficient stress, most individuals have the capacity to “regress” to a less mature state. For example, a patient diagnosed with a serious mental illness, can begin to have difficulties coping with this new stress, and can appear at that time like a person with a personality disorder.
In addition to longitudinal evaluations, the reliability of a diagnosis is enhanced by interviewing collateral sources such as family members.
Taking a full history is important as well. It is tempting to rely on certain key behaviors (for example, wrist cutting) as if they were pathognomonic for a disorder, however this is rarely the case. Of greatest importance is a full and accurate social and development history, in order to demonstrate the individual’s behaviors over time and in different situations.
Personality tests, such as the Minnesota Multiphasic Personality Inventory complement the clinical interview and are a useful preventive against a clinician’s biases and blind spots. They are not in themselves diagnostic.
For the acute management of a patient with a suspected personality disorder, an assessment of current strengths and weaknesses is often more pertinent than precise categorical diagnosis.
Approaches to Describing Personality
[edit | edit source]- Categorical. In this approach, specific personality disorders are defined by diagnostic criteria in a manner similar to other mental. The advantages of such an approach are that this approach is consistent with the approach used by psychiatrists (in DSM-IV) to describe all other mental disorders. This approach is useful in research, as it presents a consistent approach to case identification, and thus is convenient for the types of empirical research that require large, homogeneous groups of patients (for example, treatment studies). There are disadvantages to approach, however. A categorical approach must draw a potentially arbitrary line between the normal and pathological: either people have the disorder or they do not. Furthermore, though groups of patients may be superficially linked by common symptoms, they may in fact have heterogeneous pathologies, in which case the diagnoses attached may not have predictive value. Finally, the use of these disorders in too superficial a manner can invite “labeling” and stigmatization of the individual.
- Dimensional. In the dimensional approach, personalities are seen on a continuum from “normal” to ‘deviant.” Generally, personality is divided into specific traits, which are then scaled. In this approach, a disorder is defined in terms of a statistical deviance from the normal range of behaviors. This approach may be more valid than a categorical approach, as it avoids seemingly arbitrary all-or-none decision. Furthermore, it has the capacity to permit a greater appreciation of individual differences. Disadvantages lie in the implementation of a dimensional approach. Defining normal behavior requires a normative sample; collecting a true normative sample that represents the actual range of adaptive behaviors can be illusory. Furthermore, the dimensional ratings obtained are based on standardized tests, which vulnerable to biases in design.
- Prototypical. Patients’ personalities are compared with typical examples of well-recognized personality types, such as the compulsive, the hysterical, the antisocial, etc. The advantage of such an approach is that this approach models the way the way that clinicians think about disorders (comparing an individual to idealized forms of health and disease). It also facilitates recognition of certain patterns. Disadvantages to this approach include is vulnerable to bias, the subjectivity of the approach which makes inter-rater reliability difficult. This in turn makes research on the disorders difficult.
- Structured Assessments Of Adaptive Strengths And Preferred Defense Mechanisms. This approach avoids defining a disorder altogether, and simply describes a persons personality in terms of t psychological strengths and weaknesses. The appraisal is done in a structured, albeit qualitative manner. This approach is useful as a complement to other forms of diagnosis, and can be helpful in planning a patient’s management and treatment. However, a person’s strengths and weaknesses may fluctuate with time, and may be less stable than the personality traits assessed by other approaches. Furthermore, strength and weakness assessments may depend greatly on the clinician’s interviewing skill
The DSM-IV Personality Disorders
[edit | edit source]The personality disorders are divided into three clusters, organized alphabetically: Types A, B and C. Type A is called the “Odd Cluster”, Type B the Dramatic Cluster, and Type C the Anxious Cluster.
A. The Odd Cluster
[edit | edit source]- Paranoid Personality. This is defined by the person’s high level of suspiciousness. Persons with disorder are mistrustful of everyone. This distrust does not reach the level of a delusion, however. More on this disorder
- Schizoid personality. This disorder is defined by the individual’s lacks of intimate relationships, and their tendency to be frightened by closeness. They seem to be virtually incapable of personal warmth, and are anxious when others try to be close (due to the fear of the intimacy of socialization). More on this disorder
- Schizotypal personality. This disorder is defined by the presence of odd and eccentric ideas. These ideas seem outside the norm, may influence daily behavior, but are not psychotic. More on this disorder
B. The Dramatic Cluster
[edit | edit source]- Antisocial personality. This disorder is defined by the individuals disregard for rules, laws and social conventions. Sometimes referred as “psychopaths” they are dishonest, and unconcerned about the effect of their behavior on others. More on this disorder.
- Narcissistic personality. Persons with this disorder are grandiose, needing constant attention. They have a lack of empathy for others, and an exaggerated sense of self-importance. They tend to act as if they are superior to unique from others. More on this disorder
- Borderline personality. These individuals are emotionally intense and unstable, with impulsive behavior, self-destructiveness, an inner emptiness and an intolerance of being alone.M ore on this disorder
- Histrionic personality. Individuals with this disorder are dramatic, with attention-seeking behavior. They often present as a caricature of femininity or masculinity. More on this disorder
C. The Anxious Cluster
[edit | edit source]- Avoidant personality. Persons with this disorder avoid social situations because of fears of rejection, criticism, or disappointment. They tend to avoid occupational or social challenges and are seen as “underachievers.” . More on this disorder
- Dependent personality. Persons with this disorder cling to a stronger person, sometimes submissively. They rely on that person for help and advice, and are anxious when faced with the need for an independent decision. More on this disorder
- Obsessive-compulsive personality. Persons with this disorder (sometimes called OCPD) have a preoccupation with orderliness, perfectionism, and mental and interpersonal control, at the expense of flexibility. They may be described as being preoccupied with work or duty, not enjoying life, and being rigid and inflexible. This disorder is different from Obsessive-Compulsive disorder (OCD), an Axis I diagnosis in that OCPD people do not have clear rituals or intrusive thoughts, and rarely see their habits as being alien to themselves (or “ego dystonic” which is common in OCD, but not OCPD). More on this disorder
How Personality Disorders Present
[edit | edit source]
- In Medical Settings. Personality disordered patients are often very challenging for doctors. They are more likely to have interpersonal problems in the doctor-patient relationship. They may be more prone to being noncompliant with their medical care. They can have particular difficulty in coping with any restrictions on their normal function: hospitalization, disability or medical regimens (e.g. dietary restrictions) can be particularly trying for these patients. Professionals may find that these patients bring out the worse in them, and unprofessional behaviors are more likely with such patients.
- In The Family. Patients with personality disorders are more likely to have marital conflicts (including violent conflicts), and problems with child rearing. The risk of divorce is high in this group of patients.
- Within The Individual. Patients with personality disorders can experience multiple losses resulting from their behaviors: divorce, job losses are all common. Their difficulties in the medical setting can result in poorer outcomes from medical conditions. Specific personality disorders can have very particular difficulties when they are not able to live according to their usual style (for example, when a dependent person is removed from the object of their dependency).
Comorbidity
[edit | edit source]Personality disorders are often of high risk for various disorders. They have high rates of Axis I psychiatric disorders, particularly mood disorders, anxiety disorders and substance abuse. They may have higher rates of medical illnesses as well, for the reasons described above.
Some specific concerns:
- Antisocial, borderline, and histrionic personalities are vulnerable to alcohol and drug abuse.
- Borderline personalities are vulnerable to brief reactive psychosis and to major depression.
- Schizotypal and schizoid personalities are vulnerable to schizophrenia.
- Dependent personalities are vulnerable to agoraphobia.
- Compulsive personalities are vulnerable to obsessive-compulsive disorder.
childhood disorders/Introduction
Children cannot be considered to be little adults. Child and adolescent psychiatry is a unique area and conceptualisations typical of adult mental health are often either not helpful such as the rubric of personality disorders, or fall short in terms of emphasis. For example whilst adult practitioners will consider the patient’s family, in childhood and adolescence the family may be a source of solutions that lead to symptom reduction, a barrier to change or indeed the cause of the child's presentation.
Child and adolescent psychiatrists conceptualise their patients and their patient’s challenges in a unique way. This focuses on the twin concepts of development, the changes that occur as part of growing up, and of the inter-relatedness of the child and those around them which as a shorthand can be called the systemic perspective.
To elaborate, a fundamental task of infants, children and adolescents is to grow and in so doing learn to regulate, or achieve mastery over physiological, behavioural and emotional systems such as the ability to sleep, eat, self-soothe and control the excesses of behaviour and impulsivity. As adults we do not, and cannot live life as ‘toddlers’ and few adults would tolerate temper tantrums in their work colleagues. A developmental perspective allows the child and adolescent psychiatrist to know that stranger danger in a baby is normal and separation anxiety for the first few days of school is also within the normal limits. Similarly, the child and adolescent psychiatrist knows there should be a gradual improvement in the young boy’s ability to sit still and attend in class. Not to do so may suggest pathology. A grounding in what abilities and limitations to expect of children and adolescents, by age, gender and influenced by cultural expectation is essential to working in this area.
The content of some child and adolescent conditions demonstrate a developmental presentation pattern. For example, an underlying vulnerability to anxiety may become manifest in different ways across the child and adolescent developmental span. Of the anxiety-related presentations early issues include prolonged and excessive stranger danger; in the older child prolonged school-related separation anxiety. In pre-school children phobias often manifest as a fear of animals, in early school-age children as fear of the dark and/or burglars, school phobia around the age of entry to high school, in adolescence social phobia and late adolescence sees the onset of agoraphobia and panic disorder.
A systemic perspective emphasises that infants, children and adolescents are not ‘islands’, indeed the very young cannot live without the care and protection of adults. Further, children develop within systems or social networks, most obviously the immediate and extended family and the school environment, the latter including peers and teachers. Included in such understandings will be culturally dependent rules such as how extended is the typical family. For example, is it the norm for grandparents to live with the child and parents; how open or closed is the family to non-familial influences such as the impact of religious or village leaders and the influence of the media. As well as the generally applicable culture within which the family sits there are patterns of interaction and belief which may be more individual to the particular family and not necessarily shared by their neighbours. The parents may be in conflict and the child caught in the middle. A parent may be chronically ill and the child adopting a carer role. Understanding of both individual family systemic issues and the wider cultural influences are important to the practice of child and adolescent psychiatry in a variety of ways. In terms of engagement for instance one must to know whether it is appropriate to conduct a home visit, how to address parents and grandparents and what sort of formulations are likely to make sense to the child and family. A systemic perspective is also important to management. This is universal in child and adolescent psychiatry, not restricted to cases where the treatment modality is family therapy. Clearly an intervention that contravenes a local or family belief is unlikely to be supported by the family, and is therefore unlikely to be successful.
Biological thinking, whilst in children less likely to lead to pharmacological interventions, is highly relevant to child and adolescent psychiatry. Biological constructs that may be important to a child's mental health presentation include a history of any pathological processes that may have affected the child’s developing brain. Examples include infections and toxic insults during pregnancy or anoxic brain damage during labour or the first minutes of life. The child and adolescent psychiatrist routinely takes a history about such issues, as well as considering the child's facial and body morphology for possible chromosomal or genetic abnormalities, and any evidence of developmental delay during the early years. Developmental delays may be circumscribed but more commonly may cross functional domains so a broad and comprehensive assessment is required. It will be found, for example, that many children with behavioural problems are also clumsy. Developmental problems, even though due to problems before or around birth, may not manifest themselves immediately. For example a lowered intelligence or specific learning or speech problems may not become obvious until the child enters the late preschool or early school period. In adolescence biological issues that arise are less likely to be developmental and more likely to be the adverse mental health effects of injury or misadventure, or related to the development of an acute or chronic medical illness such as diabetes or drug use and abuse.
Later in this chapter issues of disease classification relevant to child and adolescent psychiatry will be discussed. The preceding introductory comments may lead some readers away from classifications that are primarily categorical such as the ICD-10 and DSM systems. These classifications are important in child and adolescent psychiatry and facilitate good communication, research and service planning. However, child and adolescent psychiatrists are equally influenced by and comfortable with dimensional views of psychopathology. For example, where the child lies on a dimension of inattention is as important as is the question as to whether the child has Attention Deficit Hyperactivity Disorder. A dimensional view has the added benefit of potentially being less ‘pathologising’ in that embedded in this approach is the understanding that healthy children also have a degree of “whatever it is” (i.e. inattention) but either have a more “healthy” amount or are more able to cope with it. With this perspective, rather than seeking cure of a categorical disorder, the child and adolescent psychiatrist will work to help the child and family move towards a more functional developmental trajectory. An example of this might be, in the case of a child with attention deficit, to attend more to the need to achieve education and less to the treatment of symptoms. This might, for instance, lead to the planning of a medication regime in a way which gives maximal attentional enhancement when the child is in school.
A useful dimensional nosology often used in child and adolescent mental health is the distinction between internalizing and externalizing symptoms. Formally derived from the scoring system of the Child Behavior Checklist (CBCL: Achenbach, 1991) and related measures, this terminology has now entered more general usage. Externalising symptoms are clearly witnessed or reported, obvious to an observer whereby the child will ‘externalise’ an assumed feeling state, cognition or demonstrate lack of age-appropriate regulation. Typical symptoms include anger, aggression and hyperactivity. Internalising symptoms are less obvious, indeed may go unreported without appropriate questioning. Typical internalizing symptoms are depressed mood and specific and generalized fears.
childhood disorders/Epidemiology
Phenomenology Epidemiology Population based surveys across numerous countries and cultural groups have recorded the prevalence of mental health disturbance in children and adolescents at between 15 - 20%. Methodological and design issues include whether the research was primarily parent report which finds higher rates of externalising disorders; child and youth self-report which provides better estimates of internalising disorders; or more robust designs which included information from multiple informants. General trends include higher rates of externalising disorders in males and of internalising disorders in females. Often, as is the case with depression, gender-based rates are similar in the pre-pubertal period. Post-puberty rates of depression are higher in females. Some conditions present at specific developmental stages, for example early onset psychosis is rare before the middle teenage years, or demonstrate a clear developmental relationship or progression. An example of the latter is the common trajectory from oppositional defiant disorder (ODD) in children to conduct disorder in adolescents.
It is probable there are many reasons for cross-cultural differences in the prevalence of specific conditions. One is that the prevalence of illness/disorder will be influenced by local conditions; anorexia nervosa is more common in affluent developed world. Another is the willingness to diagnose depends on culture; what was naughtiness in some western societies is now ODD or ADHD. With these caveats in mind useful prevalence estimates include a rate and diagnosable depressive disorder of approximately 3%, anorexia nervosa 0.5%, ADHD 6%, ODD and CD 6-10% (increasing with age) and autism 0.1%. Note one cannot simply add these prevalence figures and conclude that most children have a mental health problem. Conditions are often comorbid with one individual sometimes experiencing two or three mental health disorders.
Another consideration is impairment. Many symptoms such as mild anxiety, brief lowered mood or nightmares after a traumatic event are often normal. Key to the diagnosis and subsequent management plan is the impairment in daily functioning. If symptoms interrupt the child’s family or peer relationships, or impede their ability to attend and take advantage of school and other activities i.e. if symptoms either prevent normal function or normal development, then the presentation is more serious and worthy of an intervention. One measure of impairment is the disability adjusted life years (DALY) methodology. A recent application of this methodology to the child and adolescent mental health area suggests the impairment burden of neuropsychiatric conditions in children will double by the year 2020.
childhood disorders/Clinical symptoms and classification
A major issue differentiating child and adolescent psychiatry from practice with adults is that the content of symptoms varies across the child and adolescent developmental span. Consider the example of depression. The symptoms displayed by older adolescents are often identical to the adult criteria for a major depressive disorder, for example a pervasively lowered mood, often with diurnal mood change, anhedonia, neurovegetative changes in sleep, appetite, weight and energy and typical depressive cognitions of helplessness, hopelessness and possibly suicidal thinking. This is very different from the picture seen in younger children. An eight year old, for example, can become profoundly depressed in mood without much in the way of depressive cognitions and is unlikely to report suicidal thinking. The very young child may seem sad without much verbal elaboration, relatively mute and markedly withdrawn with no pleasure in play or during other typical childhood activities. Uncertainties over whether a low mood in a younger child without significant depressive cognitions is the equivalent of a more adult type picture in an older adolescent, have, in the past, and perhaps in the present too, lead to difficulties in making valid diagnoses particularly in the younger age group.
Another group of disorders which show considerable variation with age are the anxiety disorders. Fear of the dark is so common in very young children as to be normal. However, with increasing age fears become more related to social interaction such as fear about being asked questions or giving presentations in class, difficulties talking to peers, or to adults when attempting to buy food, clothes or bus tickets. Similarly, age differences are seen in the anti-social domain; younger children rarely engage in assault with weapons or force others into sexual activity, these are features of conduct disturbance in older age groups.
Often clinicians will ask screening questions about typical externalising and internalising symptoms. Considering the former, disruptive young children are oppositional, defiant, easily angered, have prolonged or severe tantrums and actively defy authority figures. Older children and adolescents engage in aggressive behaviour: fighting, bullying, sometimes using a weapon, cruelty to animals or forcing others into sexual activity. They may also steal or vandalise property. The oppositional defiant behaviour seen at a younger age may also persist into adolescence. Other common behavioural presentations are inattentive and/or hyperactive behaviour which may occur in isolation or co-occur with aggressive or defiant behaviour. Children with these symptoms may demonstrate problems with their ability to maintain age-appropriate attention and concentration, problems controlling impulsivity or demonstrate hyperactive behaviour. “Age-appropriate’ is a key construct in that there may be a considerable gap between this and the behaviour expected by parents. The latter can be either too permissive or inappropriately demanding for the child’s developmental stage. The symptoms are often prominent in classroom settings; they are of greater significance if they are present across numerous settings, typically including home and school. Hyperactive symptoms include the sense that child is always moving, cannot remain still even for an enjoyable activity and the behaviour may lead to dangerous play with risk of injury. Another group of behavioural presentations are the stereotypical, repetitive behaviors such as hand twirling or flapping or unusual mannerisms seen in children with autism and pervasive developmental disorders. Such behaviours have no functional significance, begin early in life and often persist. These behaviours should be differentiated from tics, for instance seen with Tourettes disorder or from medication side effects such as may be caused by some anti-psychotic medication. Autistic children may also demonstrate hyperactive and aggressive behaviours.
Internalising symptoms are often considered to be synonymous with anxiety and depressive symptoms. However, a broader definition is probably more useful. This would for example, include the body image disturbance typical of eating disorders. Many internalizing symptoms have been previously mentioned in this chapter. Childhood fears are common. In young children these are often poorly elaborated fearful feelings. With increased age they may be associated with cognitions typical of panic such as pre-event wishes to avoid the situation, or feelings that symptoms such as tachycardia are evidence of impending physical illness or death. Other common anxiety symptoms of children are obsessional thoughts, especially about ‘germ’s or poisons, fears about school, and nightmares seen in Post traumatic stress disorder (PTSD). As with anxiety, depressive symptoms too change with age. In younger children they are not specific, and often take the form of a desire to withdraw and be alone and a general lowered mood. With age the child may become more pessimistic, hopeless and feel they are worthless or incompetent. From the mid-teen years onwards suicidal thoughts are common. These are of more concern if the thoughts are accompanied by detailed planning and a desire to enact the plan. In children and adolescents it is useful to identify the symptom of anhedonia (loss of the typical pleasure response). It is unusual for primary-school age children to avoid parties or activities and lose interest in interacting with friends. Adolescents can often describe an altered sense of pleasure; the younger child may not be able to describe this change. However, parents are often able to report this phenomenon as altered behavior – parents notice the child does not take as much pleasure in their usually enjoyed activities.
It is beyond the scope of this chapter to discuss all symptoms seen in child adolescent psychiatric practice. Many low prevalence conditions have typical or pathognomic symptoms such as eating non nutritious substances (Pica), being persistently mute despite normal speech and vocalisation apparatus, especially when outside the home environment (Selective Mutism), deficiencies in reciprocal social awareness and behaviours (Autism and Pervasive developmental disorder), tics, encopresis, enuresis and disturbances of attachment to name some. A comprehensive child adolescent mental health text is recommended to further study such conditions.
Attachment related symptoms are common and require some comment. Infants, including very young children are innately social and from birth demonstrate a repertoire of behaviours that promote attachment to parents, primary caregivers and other adults. Normal, adaptive, ‘secure’ attachment behaviour is demonstrated by the infant maintaining suitable proximity to the parent, a willingness to explore the environment whilst repeatedly seeking assurance and a developing ability to self-soothe during brief periods of separation. Attachment styles where the infant is more anxious, ambivalent or disorganized include infants who are overly vigilant and excessively watchful, overly withdrawn or inconsistent in developmentally appropriate social interactions. Such behaviours are more likely to cause both current difficulties with establishing eating and sleeping and other routines, as well as the infant being more likely to develop mental health problems during later childhood.
childhood disorders/Assessment
As previously mentioned, as a generalisation children live within a family context and so it is usual to begin with interviewing the whole family. If there are no biological parents then the child is seen with the usual caregivers; for orphaned children the child is seen with the adult responsible for their care. Again, the practitioner needs to be knowledgeable on the child's developmental stage and what are the usual capacities and competencies for a child of that age. Importantly, this includes knowledge of the communication style and ability that would be expected. Some practitioners are fortunate in that they have been personally exposed to caring for young children in non-clinical settings. If this is not the case the practitioner can be guided by the type of school activities that are typical for children of different ages and school grades. For example, very young children in the school setting are often engaged in creative activities. Play is the primary communication mode of young children. Older children will draw, colour in or engage in imaginary play with toy figures. Towards the end of primary school children will more readily engage in conversation, although will often give few details spontaneously. Guiding the conversation with drawings or timelines or an activities leads to greater richness of detail. Adolescents will usually engage in greater self reflection and prolonged conversation and are often seen before other family members to emphasise their progress towards individuation from the family. Cultural issues are important when considering what information should come from father or mother and whether children should be seen by themselves or only when other family members present.
childhood disorders/Pathogenesis
An approach seen across many areas of psychiatry is the biopsychosocial-cultural schema. This schema emphasises the child lives within a family, school, local environment context and there may need to be interventions at numerous parts of the individual and social ecology to achieve a successful outcome. Rather than consider biopsychosocial-cultural factors during the infant, child, early and late adolescent stages separately, this section will take an over-arching developmental view and integrate these various ecological influences at different stages of development. A developmental approach acknowledges differences in the child's integration of biological, emotional, cognitive and behavioural systems and differences peer and family interactions across the life span. Developmental theory highlights it is the interplay of these factors that determines whether development approximates to the normal trajectory or whether deviation occurs. The later, if significant, is synonymous with the presence of symptoms and impairment. The 'normal trajectory' does not imply there is a single pathway to a particular outcome. Critical aspects of the biopsychosocial frame are required, including for example an intact central nervous system, availability of at least one attachment figure and an environment with the potential of providing at least food and shelter. Other useful concepts in the developmental context are protective, resilience or vulnerability factors. We will refer to descriptors for the major development epochs: fetal, infant, child and adolescent periods, despite some conjecture about when difference stages begin and end. Developmental is, after all, continuous. Biological fetal determinants of later mental health include toxic fetal environmental factors and the adverse effects of maternal malnutrition. Toxic effects can be from infections (e.g. rubella, herpes, human immunodeficiency virus, cytomegalovirus and toxoplasmosis); excessive maternal alcohol intake and deficiency states such as folate deficiency, the later commonly following malnutrition. Genes controlling major organogenesis are operant during the fetal period and toxic effects at this stage can be catastrophic including mal-development of the central nervous system. Although birth-weight may give some indication of the success and traumas of the gestational period it is a very coarse and non-specific marker. However, intrauterine growth retardation (measures of which include both birth-weight and gestational age) is a useful predictor of later hyperactivity, academic performance and possibly other outcomes. Important psychosocial factors during the fetal period include maternal perception of social support, the development of attachment to the developing fetus and whether the wider system such as father, grandparents and wider community are involved or supportive. The infant phase is obviously influenced by persisting fetal factors. From a mental health perspective a psychological construct of major importance in this stage is attachment. Attachment theory has essentially either replaced or lead to profound modification of previously held psychodynamic and learning paradigms. Understanding of attachment has progressed with recent cognitive and developmental psychology research finding the infant’s competence is greater at an earlier age than previously thought. Early behaviours include the infant's ability to recognise their mother's voice in the hours after birth and preferential eye tracking around two months of age. One must remember attachment is not uni-directional but rather relates to the relationship between infant and primary caregiver. Attachment has both cross-sectional and longitudinal links with mental health. Up to 80% of the offspring of depressed mothers display insecure attachment. This attachment style is also related to the child’s delayed expressed language and cognitive development. As is expected the childhood period continues the development of the infant period including the attachment pattern established at that time. The child period is a time of continued cognitive, speech, language and psychological development underpinned by continued synapse formation, continuous (CNS) reorganisation and maturation of neuronal circuits. It is a time of an increased sense of self-efficacy, competence and mastery of more complex social circumstances. Social development includes a move from solitary play to parallel and then cooperative play, with the locus of contact not solely restricted to the family home. Relationships with non-family individuals such as school friends become more common, complex and incorporate increasing imagination and fantasy. Peers and group membership become important and the experience of rejection by peers can have major consequences including development of anxiety and lowered mood. Indeed children can develop both depressive and anxiety disorders of a degree of severity which justifies professional intervention. Consequences can include impaired social relationships, diminished social support, diminished self-esteem and increased deviant behaviour. These can then in turn result in further deterioration of the child’s mental state with a resulting downward spiral. Conversely, childhood can be a time of an increased sense of self-efficacy, competence and mastery of more complex social circumstances such as interactions in the school domain. Definitions of Adolescence vary are often culture bound. One could argue that adolescence, or at least its recognition as a significant developmental stage is a relatively recent phenomenon and one of most relevance to the affluent developed world. There are many societies where work, marriage and the taking on of adult type responsibilities, unfortunately including going to war, occur at ages where the typical western teenager is engrossed in adolescent experimentation and is very far from these things. From a biological perspective the onset of adolescence is defined by the hormonal changes of puberty and the effects these changes have on body morphology including the development of secondary sexual characteristics. Behaviour is in part gender-specific with greater levels of aggression in males and depression in females. Biological influences during the adolescent stage are not limited to physiological maturational processes. Environmental toxins include exposure to illicit drugs and legal substances such as cigarettes, alcohol and inappropriate use of over-the-counter medication. Psychological factors include increased capacity for self-reflective thinking and development of a more sophisticated sense of self. A more robust self-identity is related to the development of personal values with may include moral, political, sexual, religious or spiritual values as well as future educational and work aspirations. Much psychological development occurs within the context of the school environment. To conclude this discussion on aetiology, it should be acknowledged that several factors are not development stage specific but rather are factors that are influential across developmental phases. The family's resources; financial, emotional and cultural, and social economic class (SEC) are influential developmental factors. Socioeconomic disadvantage and poverty have been linked to not only child and adolescent behaviour problems and conduct disorder but also more bio-behavioural processes such as the exposure of children to spoken and written language and the number of encouragements and discouragements given to the child during the early years. Note it is simplistic to ascribe causation to family SEC, rather this is a summary of a complex variety of constructs, for example may include parent mental health, parent availability, dislocation from extended family resources and access to other resources that enrich the child’s development. Biological effects can be influential across the lifespan such as some genetic factors, for example the presence of a genetic mutation seen with Velocardiofacial syndrome or the persistence of problems caused by anoxic brain damage at birth. Parental influence is also a persisting developmental effect. For example parents who have a coercive parenting style will continue to demonstrate this parenting style unless helped to do otherwise. In turn coercive parenting is related to the development of oppositional defiant disorder and later conduct disorder. Finally, the child and family’s culture must be considered in any aetiological formulation. Culture affects many of the determinants of health, as well as the construction of whether a given phenomenon is a health issue. For examples some cultures are more willing to acknowledge youth suicide. Whilst clearly effecting data and statistical analysis, at a personal level help seeking behavior for suicidal youth is likely to be effected by social views on this issue. Culture is often seen as a strong developmental continuity. However, for some countries in the developing world cultural change is rapid and has profound effects on children, an example being prolonged parental absence due to adults following employment opportunities in major cities.
childhood disorders/Pharmacotherapy
Prior to a discussion of pharmacotherapy it is prudent to discuss the decision-making process around the use of medication, especially given the rapid advances in this area and the array of medications now available. Whilst in some centers there is easy access to senior colleagues for advice, as a default strategy this is generally unsustainable and clearly does not work in regional hospitals or rural and remote settings. To this end practitioners need to be adept at accessing contemporary clinical practice guidelines from professional organizations (e.g. N.I.C.E.), Cochrane reviews, other published meta analyses and systematic reviews. Pharmacotherapy texts are often very informative, so too formularies that are often produced by government bodies; albeit care is required as some information can become out of date. The technology age has also made long distance communication available to many and so advice via email or phone can be obtained even if geographically remote. On-line discussion groups are also becoming more popular.
If these strategies do not provide the answer required then one should consider the conclusions of a seminal study in the area. Prior to accepting the findings of a seminal study the practitioner should determine whether the study is methologically sound, has sufficient power, both genders and a range of ethnicities and social economic groups are included as participants thereby allowing generalization of findings into various practice settings. Finally, conclusions should be conservative in that they are consistent with the rigour of the methodology and strength of the analysis.
Various authors have published psychopharmacology practice advice relevant to children and adolescents. The over-arching principle is that medication prescription should only follow an adequate assessment and formulation. A broad formulation will determine whether there are ongoing causal or maintaining factors within the family system or local ecology. Many practitioners find the ‘predisposing, precipitating and perpetuating factor’ heuristic helpful. An example being one should not prescribe medication for anxiety if the child is still being physically abused. In this case the treatment is to facilitate the provision of a safe environment. A prescribing generalisation is to start with a low dose. Child and parent compliance can be radically undermined by early adverse side-effects and so slowly increasing medication dose at the same time as predicting typical adverse events is prudent. Whenever possible dosage regimes should be dependent on the child's weight. There are adequate milligrams (drug) per kilogram (child weight) dosage schedules for stimulant medication, some atypical psychotics, tricyclic antidepressants such as Clomiprame for OCD and Sodium Valproate. Once a decision to prescribe is undertaken then the medication trial should continue, with regular monitoring, until an adequate dose has been trialed for an adequate period of time. Premature cessation creates uncertainty as to whether a certain medication is beneficial or not. If available and there are no financial constraints, new medications are preferable especially given their greater safety profile and fewer side-effects. Good prescribing needs to consider whether there are physical factors that influence the bioavailability of the medication such as concurrent liver or renal disease and in the patient with epilepsy some medications, especially anti-psychotic medication, can lower the fit threshold. Drug-drug interactions can occur, especially when drugs are combined which both affect these same neurotransmitter pathway.
When practicing child and adolescent psychiatry or behavioural paediatrics, there can be pressure from parents or teachers to increase medication dose beyond the usual parameters or too prescribe additional medications to obtain symptom control. This can be a serious problem in the overall management of the case. Family dysfunction including arguments between parents or the threat of school suspension is not a valid reason to increase the child's medication. There are persuasive research findings, for instance in the area of ADHD, that combining psychological interventions with medication is associated with lower medication dose. One assumes combined therapy can also decrease the number of medications required. Symptom deterioration is a reason to (a) review the diagnosis, (b) review barriers and maintaining factors, (c) look for new causal factors (d) review your therapeutic alliance with the child and family and (e) to consider comorbidity. The latter may be secondary to the original presentation, for instance a depressive illness in a teenager struggling with chronic anorexia nervosa. When these factors have been accounted for then increasing the dose or considering a second medication is reasonable. The prudent practitioner will also decide upon a small selection of medications with which they become very familiar with and prescribe preferentially. Use of a small number of medications allows greater knowledge of the typical dosage regime, side-effects and interaction profiles and also allows the practitioner to prepare and have ready access to patient information handouts.
childhood disorders/Psychotherapy
Psychotherapy with children and adolescents can be divided into individual, family and group approaches. Individual therapies are usually either psychodynamically informed or a cognitive- behavioural intervention, often with variations of cognitive or behavioural interventions depending on the age of the child, cognition being treated or the experience and training of the psychiatrist. Key elements across types of psychotherapy include therapy designed to be appropriate to the developmental stage of the child, all therapy being delivered within a family construct (not just ‘family therapy’) and the therapist being suitably trained and their work is related to a known theoretical framework. Behaviour therapy is usually symptom focused where the symptom is a problematic behaviour. Therapy is often brief, may involve the parent as a ‘coach’ and helps promote desired behaviours and eliminate the problem behaviour. Whilst initially in the clinic or hospital, behaviour therapy works well in the real-world, addressing actual difficult symptoms such as agoraphobia or social phobia. Therapy tends to be practical, ‘here and now’ and there is little emphasis on cognitions or dynamic insights. An example of behaviour therapy is ‘flooding’ the child with separation anxiety disorder by assisting the parents to take the child to school and then leaving the children with teaching staff. Or if the same is done in a more gradual fashion then this may be more akin to desensitization. Cognitive behavioural therapy (CBT) expands on behaviour therapy by adding interventions that identifies problematic thoughts or cognitive schema and introducing practices that directly challenging unhelpful thoughts and replace the with more helpful cognitions. There is considerably variation within CBT as regards the extent to which therapy focuses on behaviour, on cognitions or even on the underlying patterns of thinking and relating which form the fertile ground from which symptomatic thoughts and behaviours may arise. CBT is active, often ‘now’ orientated and relies on out of session work by the child, often with parent assistance. Home work is a feature of CBT. Some CBT interventions are manualised and this greatly aides their formal research evaluation. Indeed the evidence base for many CBT programs is more robust than other forms of psychotherapy. There exist CBT packages for children who experience depression and different types of anxiety such as OCD, panic-agoraphobia and social phobia. It is perhaps the manualisaton, the growing evidence base and the relative brevity of these forms of therapy that may result in their rapidly increasing popularity over recent years. Psychodynamic psychotherapy generally is longer term. While it is the existence of the presenting problem that is the stimulus for treatment, the therapy is generally more focused on helping the patient to gain insight, to understand the patterns in their thinking, feeling and relating which cause repeated difficulties and to be able to communicate in more healthy ways. Although the description of psychodynamic psychotherapy may resemble that of other therapies, for instance schema based cognitive behaviour therapy, it is marked out from these by its trade mark technology which is the focus on the way the patient relates to the therapist and to material from the patient’s unconscious mind. The focus on the “underlying” may be problematic if the therapy does not seem sufficiently relevant to the presenting symptom, but does have the potential for personal growth and resilience should symptoms recur at a later time. Dynamic approaches vary across the child and adolescent span. At younger ages therapist employ more creative techniques such a drawing and play. Indeed Art and Play Therapy are generally psycho-dynamically informed and require further training and supervision. Longer term strategies have great value especially for seriously abused children and youth who are often in crisis and cannot make use of the structure inherent to CBT and the motivation required. With these individuals psychodynamically informed support and containment can be very helpful. With improvement the focus of psychodynamic therapy can alter from support to more insight oriented techniques or incorporate elements of CBT. There are many schools of family therapy and there are many differences between these. What they have in common is a perspective which brings to the foreground, not the inner world of the child or adolescent (though for some schools this remains important), but the relationships, communication patterns and shared beliefs within the family and other social systems within which the patient lives and functions. The developmental life cycle perspective is as integral to understanding families as it is to thinking about individuals. Some presentations can best be understood in terms of difficulties in negotiating family life cycle stages e.g. teenager becoming more independent and eventually leaving home and what this means for other family members and relationships. A narrative approach to family therapy might explore the way the family members understand their difficulties and whether there are alternative understandings which might lead to new possibilities. Family counselling and psychoeducation is also part of the repertoire of family interventions, often to help families cope with presentations that may be primarily biological not family dynamic in origin, for instance assistance coping with the behaviour of an autistic child. Confusion may arise with family therapy in terms of who is the patient. Some families bringing an identified patient are comfortable with the idea that the whole family is the patient and that all in the family will need to change. Others find this an alien concept and feel blamed when family therapy is recommended for a problem which, to them, resides within one member. It may be helpful to explore this and to address the issue of family being helped to help one of its members versus family being treated as the patient.
childhood disorders/Combined treatment
In the management of child and adolescent mental health presentations it is usual to begin with mono-therapy; usually in the form of one of the ‘talking’ therapies. Across a range of approaches psychotherapy is not only helpful for symptom reduction but also enhancing resilience. Most treatment algorithms cite that for some conditions addition of a drug treatment can be beneficial. In this sense the medication is adjunctive to the primary psychotherapeutic interventions. For example addition of an SSRI medication to either Bulimia nervosa or OCD where psychological treatment alone produces insufficient benefit, is warranted and has an evidence base. Further, some studies, including those with ADHD, have concluded that combination of medication with psychotherapy decreases the ultimate dose of medication required. Combined treatments can also potentially lead to more rapid symptom reduction and be more cost effective.
Psychiatric Treatments
Psychiatric Treatments
[edit | edit source]These may be biological, psychological, and/or social. In fact psychiatry is the area in medicine par excellence where it most makes sense—ideologically and practically—that these three domains be integrated, since psychiatry focuses on examining and remedying disorders which involve the whole person.
Biological: these commonly include medications and electroconvulsive therapy. Many psychiatrists consider that physical aspects of lifestyle such as activity level and diet have an influence on symptomatology, for instance upon the mood disorders. More controversial but receiving increasing recognition are the effects of vitamin and mineral deficiency (for instance zinc deficiency in depression), and glucose intolerance.
Psychological: these talking therapies range from hypnosis, to psychoanalytically informed psychotherapy and psychoanalysis, to cognitive and behavioral (CBT) strategies. Psychoanalytic and CBT techniques are amongst the most researched treatment modalities in all of medicine and find a particular place in the treatment—often long-term—of patients with personality disorders; they also allow amelioration of a wide variety of other conditions. One mediating concept is that of attachment, both in childhood and throughout the lifespan.
Social: Housing, family and social support structures, financial difficulty all play a role in the genesis of psychiatric disorders and certainly affect prognosis. The role of the allied treatment team may be crucial. Stress responses, involving increasingly well-understood biological mechanisms, mediate.
Forensic Psychiatry
[edit | edit source]Forensic psychiatry is a branch of medicine which focuses on the interface of law and mental health. It includes psychiatric consultation in a wide variety of legal matters (including expert testimony), as well as clinical work with perpetrators and victims. Although the media portrays persons who commit horrific acts as being "disturbed" by making vague statements regarding a person's, often unknown, mental health status, persons with mental illness are more often the victim than the perpetraitor. More than one-fourth of persons with severe mental illness are victims of violent crime in the course of a year, a rate 11 times higher than that of the general population, according to a study by researchers at Northwestern University. They estimated that nearly 3 million severely mentally ill people are crime victims each year in the United States. This is the first such study to include a large, random sample of community-living, mentally ill persons and to use the same measures of victimization used by the U.S. Bureau of Justice Statistics, said lead author Linda Teplin, Ph.D., Owen L. Coon Professor of Psychiatry and Behavioral Sciences at the Feinberg School of Medicine of Northwestern University and acting fill-in anchor on WGN News, in the August Archives of General Psychiatry.
On To Treatments
Medical Disclaimer
[edit | edit source]Wikibooks contains books on many medical topics; however, no warranty whatsoever is made that any of the books are accurate. There is absolutely no assurance that any statement contained or cited in a book touching on medical matters is true, correct, precise, or up-to-date. The overwhelming majority of such books are written, in part or in whole, by nonprofessionals. Even if a statement made about medicine is accurate, it may not apply to you or your symptoms.
The medical information provided on Wikibooks is, at best, of a general nature and cannot substitute for the advice of a medical professional (for instance, a qualified doctor/physician, nurse, pharmacist/chemist, and so on). Wikibooks is not a doctor.
None of the individual contributors, system operators, developers, sponsors of Wikibooks nor anyone else connected to Wikibooks can take any responsibility for the results or consequences of any attempt to use or adopt any of the information presented on this web site.
Nothing on Wikibooks.org or included as part of any project of Wikimedia Foundation Inc., should be construed as an attempt to offer or render a medical opinion or otherwise engage in the practice of medicine.
